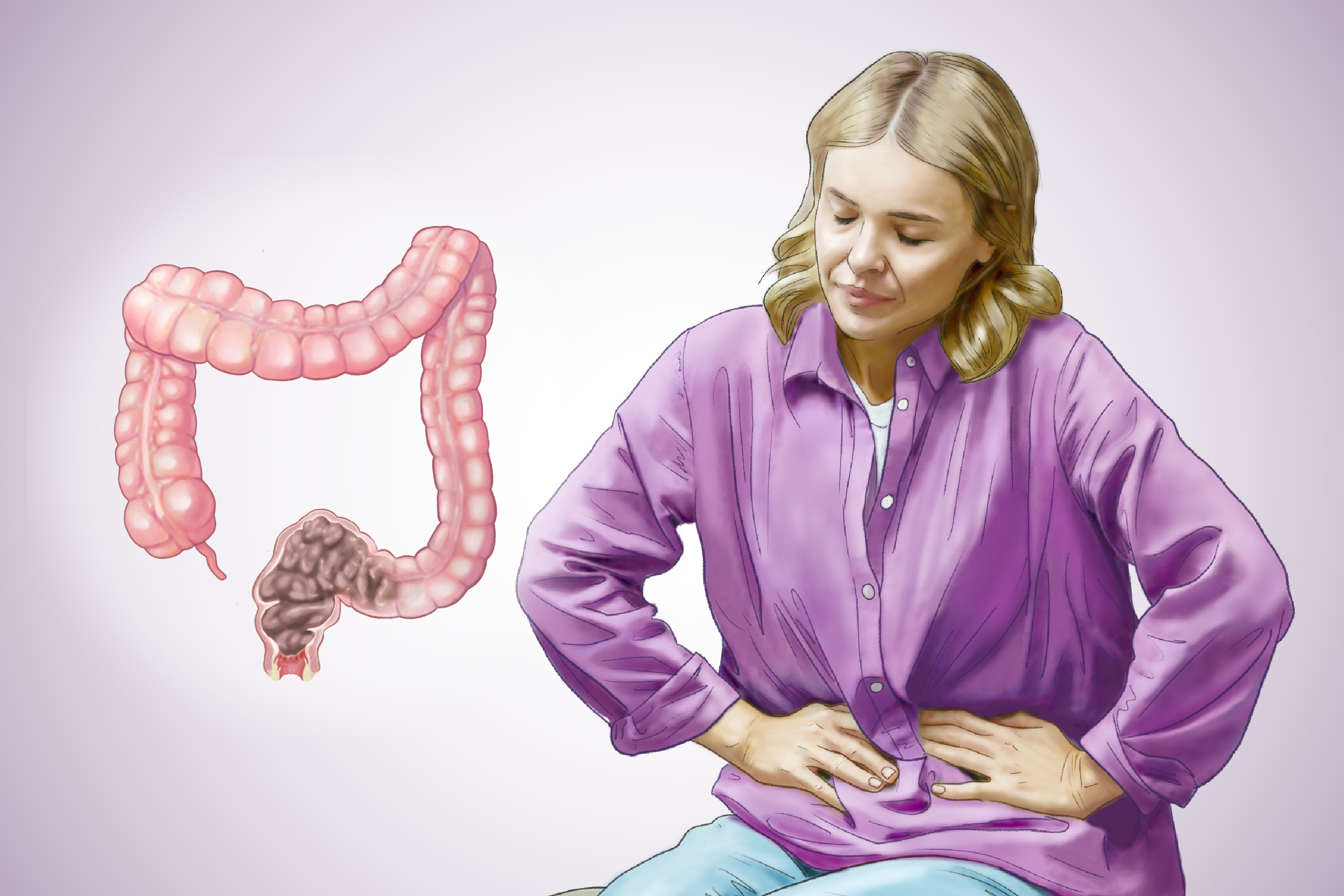
Common Symptoms
Some frequently seen symptoms include:
- Infrequent bowel movements, such as passing stools less often than usual
- Straining or pain when passing stool
- Small, hard, pellet-like stools
- Leaking small amounts of watery stool
- Bloating and a firm or swollen abdomen
- Stomach pain or cramping
- Excessive gas or frequent burping
- Loss of appetite due to feeling uncomfortably full
- Pressure or fullness in the rectum
- Nausea or vomiting
When to See a Doctor
Some symptoms suggest a more serious problem and require medical attention, including:
- Blood in your stool, either bright red or dark
- Unintentional weight loss
- Fever above 100.4 degrees, which is unusual with constipation, and may signal a complication
- Persistent nausea or vomiting
- Signs of anemia, such as fatigue or weakness
- Abdominal pain that doesn’t improve after a bowel movement or wakes you from sleep
- Rectal pain
- Inability to pass gas
- Lower back pain caused by the stool pressing on nerves
Chronic Constipation Symptoms
You may have chronic constipation if constipation lasts for at least three months, and you experience two or more of the following symptoms:
- Straining during more than 25 percent of bowel movements
- Hard stools in more than 25 percent of cases
- A feeling of incomplete evacuation in more than 25 percent of cases
- Fewer than three bowel movements per week
Also, if lifestyle changes such as increasing fiber, exercise, and hydration don’t relieve constipation, it may be chronic.
Common Lifestyle Causes
These are the most frequent culprits behind constipation and the easiest to address:
- Bathroom Habits: Ignoring the urge to have a bowel movement or not maintaining a regular bathroom routine
- Diet: Eating too little fiber, drinking too little water, consuming too much coffee, tea, or alcohol, or eating too little overall
- Physical Activity: Living a sedentary lifestyle or not exercising regularly
- Lifestyle Changes: Traveling, which can disrupt normal routines
- Laxative Overuse: Using laxatives frequently, which can lead to dependence and make natural bowel movements more difficult
Emotional Factors
Your gut and brain are closely connected, and mental health significantly affects digestive health:
- Stress: Disrupts normal digestive function and can trigger constipation or diarrhea; often linked to anxiety from work or personal problems
- Depression: A common physical symptom of depression, as emotional state affects bowel function through the gut-brain connection
Medical Causes
When constipation isn’t related to lifestyle, it may stem from:
- Anatomic Causes: Structural abnormalities in the digestive tract, including anal stenosis or atresia, anal fissures, anteriorly displaced anus, imperforate anus, thrombosed hemorrhoids, intestinal strictures, obstructing tumors, and anal strictures.
- Abnormal Musculature: Disorders affecting muscle development or function, such as prune belly syndrome, gastroschisis, Down syndrome, and muscular dystrophy.
- Rectocele: A condition in which the rectum bulges into the weakened back wall of the vagina, especially during straining or bearing down.
- Hernia: An abdominal hernia that decreases effective intra-abdominal pressure, making bowel movements more difficult to pass.
- Hormonal and Metabolic Conditions: Hypothyroidism (underactive thyroid), diabetes, and imbalances in calcium or potassium levels.
- Digestive System Disorders: Irritable bowel syndrome, inflammatory bowel disease, Crohn’s disease, ulcerative colitis, celiac disease, structural problems such as anal tears, hemorrhoids, intestinal narrowing, or tumors, and pelvic floor dysfunction.
- Disordered Defecation (Dyschezia): A condition in which the bowels cannot generate enough force to push stool out of the rectum, or the muscles around the rectum and external anal sphincter fail to relax properly during bowel movements.
- Neurological Conditions: Parkinson’s disease, multiple sclerosis, stroke, spinal cord injuries, or defects.
- Other Conditions: Certain cancers, including colon, rectal, ovarian, and brain cancers; chemotherapy treatment; cystic fibrosis; scleroderma (autoimmune disorder); and cow milk protein allergy, especially in children.
- Medications: Pain medications, particularly narcotics, and certain antidepressants, as well as many blood pressure medications and drugs used to manage Parkinson’s disease or seizures; antacids containing aluminum or calcium; nonsteroidal anti-inflammatory drugs such as ibuprofen; and dietary supplements including iron, calcium, or vitamin D taken in excessive amounts. Both very low and very high vitamin D levels may affect bowel function, with an imbalance in either direction contributing to constipation.
Other factors can include the following:
- Pregnancy: Hormonal changes, reduced physical activity, and pressure from the growing uterus on the intestines
- Advancing Age: Older people may experience decreased intestinal muscle activity and increased medication use
- Abdominal X-Ray: Shows whether the bowels are filled with stool or excess air, helping assess stool buildup or blockage
- Blood Tests: Check for conditions such as iron-deficiency anemia, which may indicate slow or hidden bleeding in the colon
- Lower Gastrointestinal Series (Barium Enema): Uses X-rays and a contrast liquid called barium to visualize the rectum and intestines and identify narrowing, blockages, or structural problems
- Defecogram: Assesses stool control and evacuation
- Colonoscopy: Examines the entire large intestine to detect abnormalities such as inflammation, ulcers, bleeding, or growths
- Sigmoidoscopy: Examines the lower part of the large intestine to help determine causes of constipation
- Colorectal Transit Study: Measures how long stool takes to move through the colon using X-ray-visible markers
- Anorectal Function Tests: Evaluate how well the anus and rectum function and whether constipation is related to muscle or coordination problems
- Fecal Immunochemical Test: Detects hidden blood in the stool
1. Dietary Fiber and ‘Natural Laxatives’
For decades, increasing dietary fiber has been a standard recommendation for relieving constipation. Most adults have been advised to eat at least 25 grams of fiber per day, depending on age and gender. Fiber comes in two forms—soluble and insoluble—both of which play roles in digestion. Soluble fiber absorbs water and forms a gel that can soften stool, while insoluble fiber adds bulk and helps stool move through the digestive tract.
- Prunes: Eating prunes or drinking prune juice may help relieve constipation because they contain fiber and sorbitol, a natural sugar alcohol with mild laxative effects
- Apricots: Stewed apricots may help promote bowel movements when softened and eaten regularly
- Kiwis: Kiwis contain actinidin, an enzyme that helps speed digestion by breaking down proteins more efficiently
- Apple Juice: Apple juice contains smaller amounts of sorbitol and may be a helpful alternative for people who do not tolerate prunes
- Olive Oil: Taking a teaspoon of olive oil on an empty stomach in the morning may help lubricate the digestive tract and soften stool
- Hot Beverages: Drinking warm beverages, especially caffeinated drinks like coffee or tea, may stimulate bowel movements and speed digestion
The following foods and diets should be avoided:
- Very low-carbohydrate diets, such as the keto diet, are often high in fat and low in fiber
- Foods high in refined sugars, including heavy desserts, may increase the risk of constipation
2. Fiber Supplements
Dietary fiber offers many health benefits, but only a small percentage of people meet the recommended intake levels through food alone. For those with low-fiber diets, fiber supplements can help improve regularity. Fiber supplements generally work gradually and may cause gas or bloating, so adequate fluid intake is important.
3. Probiotics
Probiotics are beneficial bacteria and yeast that help maintain a healthy balance of gut microbiomes. They may support regular bowel movements by improving stool consistency and promoting normal gut motility. Dietary sources include live-culture yogurt, kefir, and yogurt drinks.
4. Sufficient Liquids
Staying well-hydrated is essential for relieving and preventing constipation because fluids help fiber work effectively and keep stool soft and bulky by making it easier to pass.
5. Physical Activity
Regular exercise helps improve bowel motility by stimulating the natural contractions of intestinal muscles, allowing food to move through the colon more efficiently. Aerobic activities such as brisk walking or cycling are especially effective. Any amount of regular physical activity is beneficial, particularly for people with limited mobility.
6. Kegel Exercises
Pelvic floor, or Kegel, exercises help strengthen the muscles that support the bowel, rectum, and anus, which may improve bowel control and ease bowel movements.
7. Relaxation and Music Therapy
A May 2025 study involving more than 600 recruits found that short-term progressive muscle relaxation combined with music therapy may help improve gastrointestinal symptoms, including constipation.
1. Laxatives
Laxatives are medications that help promote bowel movements. They come in different types, each working in a distinct way on the digestive system. In some cases, different types of laxatives may be combined based on individual needs and response.
- Bulk-Forming Laxatives: Often the first laxative option recommended, these help stools retain water, making them softer and easier to pass and reducing the risk of fecal impaction. Common plant-based examples include ispaghula husk, sterculia, and methylcellulose.
- Osmotic Laxatives: Used when stools remain hard despite bulk-forming laxatives, these draw water into the bowel to soften stool and stimulate bowel movements. Common examples include lactulose and macrogols. There are four main types: saline laxatives, which work within 30 minutes to 3 hours; lactulose, which works over 6 hours to two days; polymer laxatives such as polyethylene glycol, which typically act within 6 hours; and glycerine suppositories, which soften stool and may also stimulate bowel movements.
- Stimulant Laxatives: Used when stools are soft but difficult to pass, these stimulate the muscles of the digestive tract to move stool through the colon more effectively. Common examples include senna, bisacodyl, and sodium picosulfate, and they typically act within 6 to 12 hours.
- Stool Softeners: Products such as docusate add moisture to stool to make it easier to pass.
- Lubricants: Lubricants such as mineral oil help stools pass more easily and may be useful for low bowel blockages, anal fissures, or painful hemorrhoids. However, they should not be used for more than one week, as prolonged use may lead to vitamin deficiencies or interfere with medications. Mineral oil is not recommended for pregnant women or for people who have difficulty swallowing, and oral mineral oil carries a risk of pneumonia if it enters the lungs.
- Fruit lax: Dried fruit spread may also help ease constipation. You can find various recipes for it online.
For short-term constipation, pharmacists usually advise stopping laxatives once stools are soft and easy to pass. For long-term use, laxatives are gradually reduced rather than stopped abruptly. When multiple laxatives are used, the dosage of each is typically tapered one at a time, which may take several months.
2. Suppositories
Suppositories are small, solid medications that are inserted directly into the rectum, where they dissolve and work to relieve constipation. They may function as lubricants or stimulant laxatives by encouraging bowel muscles to contract and move stool along. Suppositories are often used for children or people who have difficulty swallowing oral medications and provide fast and targeted relief.
3. Other Medicines
Other medications may relieve constipation in different ways, including:
- Enterokinetics: Medications such as prucalopride work by stimulating serotonin (5-HT4) receptors in the digestive tract to increase intestinal muscle movement and improve bowel motility. Common side effects include nausea, diarrhea, abdominal pain, and headache.
- Guanylate Cyclase-C Agonists: Drugs such as linaclotide increase fluid secretion in the intestines, making stool easier to pass and improving related symptoms.
- Peripherally Acting Mu-Opioid Receptor Antagonists (PAMORAs): PAMORAs, such as methylnaltrexone, naloxegol, and naldemedine, treat opioid-induced constipation when other treatments haven’t worked. Alvimopan is another option, but it is used only short-term in hospitals to help treat postoperative ileus, a temporary slowing of the intestines after surgery.
4. Enemas
An enema involves inserting liquid, usually water, sometimes with salt, into the rectum through the anus. The liquid loosens stool and stretches the rectal walls, triggering muscle contractions that produce an urgent bowel movement.
5. Transanal Irrigation
Transanal irrigation is a structured method for emptying the lower bowel using a catheter or specialized device to flush water into the rectum. Unlike a regular enema, transanal irrigation can empty the entire lower bowel, making it particularly useful for people with chronic constipation. Training from a health care professional is required to use the equipment safely.
6. Manual Defragmentation
Fecal impaction, in which hard stool becomes stuck in the rectum, is usually treated first with enemas, starting with tap water and then small amounts of specialized solutions. If this approach doesn’t work, a doctor may need to manually break up and remove the stool. This procedure can be painful, so local anesthetic creams or, in some cases, sedation may be used to reduce discomfort.
7. Sacral Nerve Stimulation
Sacral nerve stimulation has been used to treat constipation that does not respond to other treatments by helping regulate the nerve signals that control the large intestine. It has been shown to improve bowel movement frequency in some children with functional constipation, but in many patients, the benefits lasted less than six months.
8. Biofeedback
Biofeedback therapy trains people to better coordinate their rectal and abdominal muscles for more effective bowel emptying. Using gentle electrical signals, it helps increase awareness of muscle activity and improve control. Biofeedback is often used alongside dietary improvements to help relieve chronic constipation.
9. Cognitive Behavioral Therapy (CBT)
A 2022 study showed that combining CBT with biofeedback improved constipation symptoms, depression, and anxiety more effectively than biofeedback or standard treatment alone. About 67 percent of patients receiving both therapies were able to fully relax their bowel muscles during treatment, compared with none of those receiving only biofeedback or standard care therapy.
10. Surgery
Surgery is rarely used to treat constipation, but may be considered for specific conditions such as a large rectocele, in which the rectum bulges and traps stools, or rectal prolapse, when the rectum slips out of its normal position and interferes with bowel function. Pelvic floor surgery can help repair these issues, although some people may develop new symptoms afterward, including diarrhea, bowel obstruction, or incontinence.
11. Abdominal Massage Therapy
A 2023 meta-analysis found that abdominal massage therapy may increase bowel movement frequency, make stools easier to pass, improve stool consistency, and enhance quality of life for people with constipation.
12. Acupuncture
A 2020 meta-analysis suggested that acupuncture may be a safe and effective treatment for functional constipation, improving bowel movement frequency, stool consistency, symptoms, and quality of life, although more high-quality studies are needed.
- Establish a Routine: Use the restroom at the same place and time each day, allow enough time, and respond promptly to the natural urge to have a bowel movement rather than delaying it.
- Change Posture: Place your feet on a low stool so your knees are higher than your hips, which can help straighten the rectum and make stools easier to pass.
- Time Meals: Eat small meals and snacks throughout the day to stimulate gut activity and promote more regular bowel movements.
- Track Habits: Keep a record of your food and drink intake, activity levels, and bowel movements to help identify patterns or triggers for constipation.
- Hemorrhoids: Repeated straining can damage the blood vessels in the rectum, causing swollen veins.
- Rectal Bleeding: Frequent straining leads to bleeding from hemorrhoids or anal fissures.
- Stercoral Ulcer: Impacted stool can wear away the lining of the lower bowel, potentially causing bleeding or bowel perforation.
- Rectal Prolapse: Persistent straining can push part of the rectum through the anus.
- Urinary Incontinence: Constant straining weakens the pelvic floor muscles and increases urine leakage, especially during coughing, laughing, or sneezing.
- Fecal Impaction: Stool becomes tightly packed in the colon or rectum, sometimes causing leakage around the blockage.