“Supporting the gut microbiome can help reduce colorectal cancer risk and may even enhance prevention and treatment,” Sachin Aryal, gut microbiome researcher at the University of Toledo, told The Epoch Times.
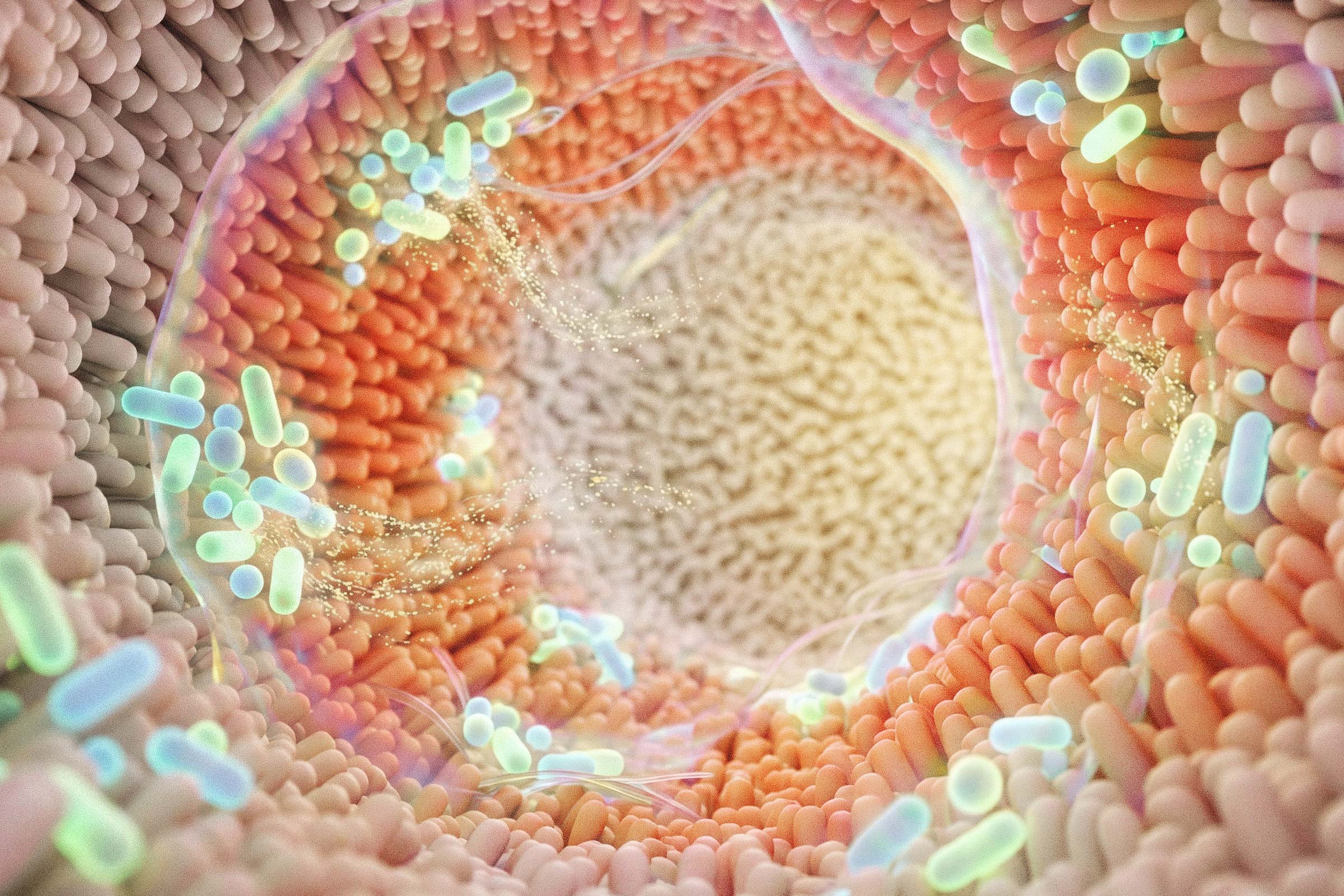
The microbiome has been linked to many aspects of health and has been shown to also play a key role in colorectal cancer.
The good news is that the microbiome is not fixed and that it can be influenced by everyday habits and choices.
How Gut Bacteria Influence Colorectal Cancer
“We’re learning that the bacteria in the gut matter more than we used to think,” Dr. Cedrek McFadden, colorectal surgeon and medical advisor to the Colorectal Cancer Alliance, told The Epoch Times.
Gut bacteria are not just sitting there as bystanders. They interact directly with the lining of the colon, the immune system, and inflammatory processes over time. When the microbial balance is off—a condition called dysbiosis—some bacteria can create a low-level inflammatory state or produce substances that irritate the colon lining. Over many years, that kind of environment can contribute to cancer, McFadden said.
Because the colon is directly exposed to gut bacteria and their by-products, colorectal cancer appears to be more strongly influenced by the microbiome than many other types of tumors, although the microbiome can also affect other cancers indirectly.
“It’s not that one bacterium causes cancer,” McFadden said. “It’s more about the overall balance and what the colon is being exposed to day after day.”
When dysbiosis continues, it can further damage the gut barrier—a condition sometimes referred to as “leaky gut.” The tight connections between gut cells loosen, allowing bacteria and their by-products to move deeper into the gut wall. This keeps the immune system in a constant state of activation and inflammation, Raz Abdulqadir, researcher in microbiome and colorectal cancer at Penn State College of Medicine, told The Epoch Times.
“As a result, inflammatory cells release molecules that increase oxidative stress and can damage DNA in colon cells, raising the risk of abnormal cell growth,” he said.
It’s now clear that gut bacteria influence not only inflammation linked to tumor formation, but also how well the immune system recognizes and attacks cancer cell. This explains why patients with different gut microbiomes can respond very differently to the same cancer treatments.
Bacterial Culprits Identified
Several microbes have been consistently associated with colorectal cancer, including
Fusobacterium nucleatum, enterotoxigenic Bacteroides fragilis, Enterococcus faecalis, and certain strains of E. coli, Aryal said.
Fusobacterium nucleatum, for example, is found in much higher amounts in people with colorectal cancer compared to healthy people and is particularly abundant in tumor tissue. Higher levels of this bacterium are also linked to stronger inflammatory signals in the gut and can attach directly to the gut lining using a specialized protein, which helps kick-start cancer-related changes.
“However, we still need well-designed intervention studies to determine whether these microbial changes are true drivers of cancer or simply a consequence of the tumor environment,” Aryal said.
The microbiome’s impact is not only about which bacteria are present, but also what they are doing. Microbial by-products—substances produced by microorganisms such as bacteria as a result of breaking down—and toxins—such as chemicals made by bacteria that can irritate the gut or damage cells—either protect the colon or increase inflammation and DNA damage.
“This is why the microbiome is becoming an increasingly important part of conversations around early detection, prevention, and personalized cancer therapy,” Aryal said.
What You Can Do
Maintaining a healthy gut microbiome is a key factor in preventing colorectal cancer.
Dietary fiber, probiotics, prebiotics, synbiotics—products combining probiotics and prebiotics—and even fecal microbiota transplantation can help rebuild microbial balance and regulate immune and inflammatory pathways, Abdulqadir said.
Focus on Fiber and Whole Foods
From a dietary perspective, the most important step is to consistently follow an eating pattern that supports microbial diversity, especially one rich in dietary fiber. A high-fiber diet that includes fruits, vegetables, fermented foods, and prebiotic or probiotic sources helps maintain a healthier microbial balance and creates a gut environment less supportive of tumor development, Aryal said.
“Incorporating Mediterranean-style eating patterns is especially helpful because they emphasize whole grains, legumes, vegetables, and healthy fats that support microbial diversity,” he added.
Consider Targeted Supplements
Probiotics may help lower the risk of colorectal cancer. One well-studied strain, Faecalibacterium, has been shown in animal research to reduce gut inflammation and protect against colitis.
Other probiotics, including certain Lactobacillus and Bifidobacterium strains, help strengthen the gut lining and support healthy cell growth—especially in people with a history of polyps—small growths on the lining of the bowel that can sometimes turn into cancer.
“When probiotics and prebiotics are used together as synbiotics, they help reduce inflammatory mediators and create a gut environment less favorable for tumor development,” Aryal said.
Doses and specific types can vary, so it’s best to talk to a doctor before trying them.
Stay Active
Regular physical activity also plays an important role in optimizing the gut microbiome and lowering colorectal cancer risk, Aryal said.
“Exercise increases microbial diversity, enhances short-chain fatty acid production, and reduces inflammation, all of which help keep the colon healthy.”
Keep It Simple
Gut health doesn’t need to be complicated, McFadden said. His top advice is not to overthink it.
“Eat real food more often. Get fiber in your diet. Cut back on heavily processed foods when you can and don’t chase supplements or trends,” he said.
In his own life, McFadden keeps things simple. He tries to eat balanced meals, stay active, and get decent sleep. He pays attention to stress because of his awareness of its effects on the body, including the gut.
“I’m not perfect, and I don’t expect my patients to be either. I just try to be consistent most of the time.”