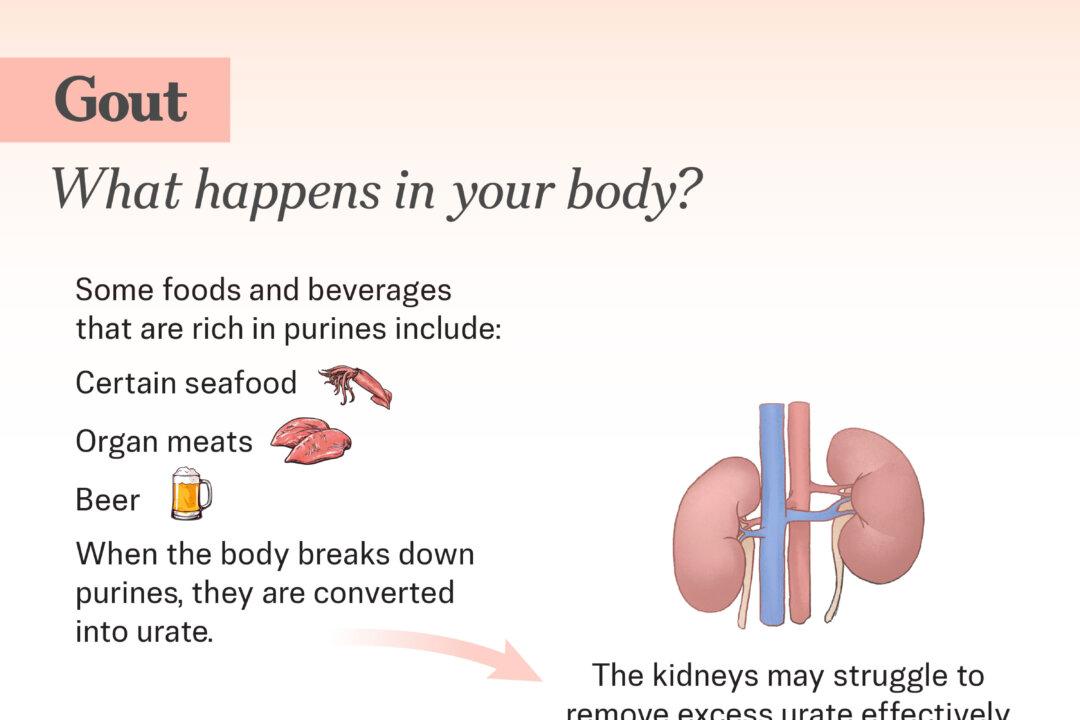
- The Body Produces Too Much Urate: About 10 percent of people naturally create excessive amounts of urate when breaking down purines. Certain conditions, such as blood cancers and rare genetic disorders, can accelerate this process.
- The Kidneys Can’t Eliminate Urate Efficiently: Even when urate production is normal, the kidneys may struggle to remove it effectively, which happens in 90 percent of cases. As urate accumulates in the blood, it eventually reaches a level where it can no longer stay dissolved.
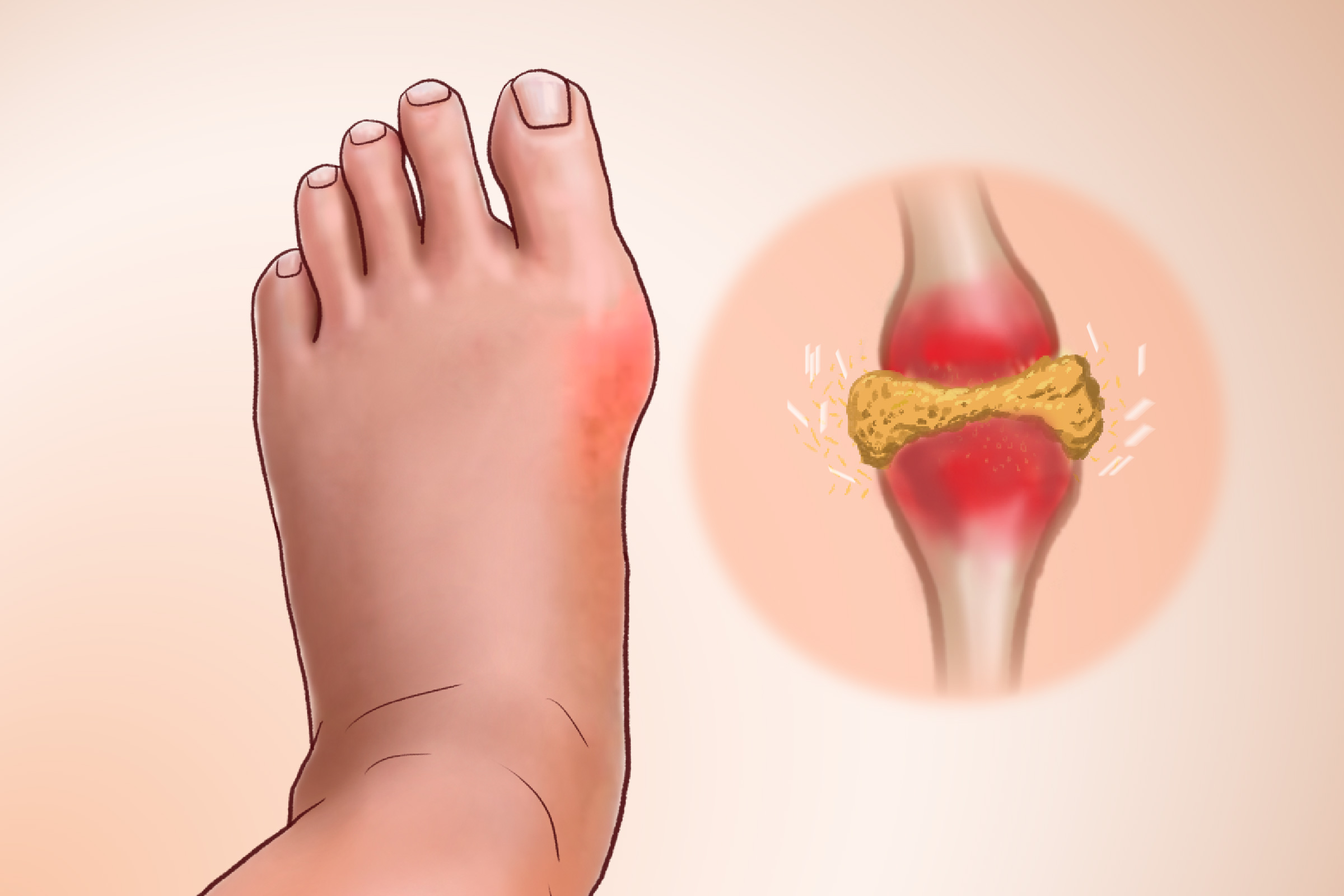
When urate levels become too high, the excess crystallizes into sharp, needle-shaped monosodium urate crystals. These crystals settle in and around the joints—most commonly in the big toe—where they trigger intense inflammation and pain.
Lifestyle Factors
These factors primarily trigger flares and increase urate levels:
- Diet: Foods and drinks high in purines—such as red meat, seafood such as shrimp and oily fish, dried beans, organ meats such as liver, and sugar-sweetened beverages—can raise urate levels and increase gout risk. High-fructose corn syrup, found in soft drinks and many processed foods, is particularly problematic, while low dietary intake of dairy products may also contribute by reducing uric acid removal.
- Beer: People who drink two or more beers a day are more than twice as likely to develop gout compared with nonbeer drinkers, since beer is high in purines. Other alcoholic drinks can also increase the risk, but to a lesser extent than beer.
- Weight: People who are overweight or obese have a higher risk of developing gout and tend to get it at a younger age. Excess weight raises urate production and inflammation, increasing the risk of urate crystal buildup and gout. Being obese nearly triples your chance of getting gout compared with someone of normal weight.
- Niacin Supplements: High-dose niacin (vitamin B3) supplements may raise uric acid levels.
Medical Conditions
Several medical conditions increase the risk of gout, including kidney disease, which reduces the kidneys’ ability to remove urate; diabetes, where insulin resistance limits urate excretion; and metabolic syndrome, a cluster of high blood pressure, high blood sugar, abnormal cholesterol, and excess abdominal fat. Blood disorders such as leukemia and other blood cancers raise gout risk through rapid cell turnover, which releases purines. Sickle cell disease and other anemias also increase gout risk by boosting urate production through accelerated red blood cell breakdown. Anemia has been linked to roughly a twofold higher gout risk, independent of kidney function.
Certain Medications and Supplements
Examples include diuretics, cyclosporin, low-dose aspirin, ethambutol, beta blockers, vitamin B3 supplements, and pyrazinamide.
Imbalanced Gut Microbiome
Because the gut microbiome helps regulate the immune system, its imbalance is linked to inflammation and may contribute to arthritis.
Other Factors
These risk factors relate to genetics, age, and other aspects of life that people cannot change.
- Genetics: Gout is influenced by many genes, each contributing a small increase in risk. Most of these genes are involved in controlling urate levels, especially by transporting urate in and out of the kidneys. Some genes affect sugar metabolism or the transport of other small molecules, while the roles of a few are still unknown. Among all identified genes, SLC2A9 and ABCG2 have the strongest effect on urate levels and gout risk.
- Family History: Having a close family member with gout increases a person’s likelihood of developing the condition.
- Gender: Men are more prone to developing gout, with a male-to-female ratio of 3:1, partly due to the lack of protection from estrogen.
- Age: The risk increases with age, especially in women after menopause, when lower estrogen levels reduce urate removal and lead to higher urate levels. Younger women rarely have gout.
- Ethnicity: African Americans or Asian Pacific Islanders have a higher risk than average.
Triggers of Gout Attacks
Urate crystals are like sparks waiting to ignite. They can remain in the joint for years without causing symptoms, but when enough crystals build up, or a trigger occurs, inflammation suddenly starts. Common triggers include:
- A Sudden Increase in Urate Levels: When urate levels rise quickly, crystals are more likely to form in the joints, which can set off a painful gout attack.
- Injuries or Trauma to the Joint: Local trauma disturbs urate crystals already sitting in the joint, triggering an inflammatory immune response.
- Excessive Intake of Purine-Rich Foods or Beverages: A sudden excess of purines raises blood urate levels and promotes crystal formation.
- Stress: Stress hormones, such as cortisol, can raise urate levels and increase inflammation
- Dehydration: Dehydration concentrates uric acid in the blood and joints, increasing crystal formation and precipitation.
- Fatigue: Fatigue is often associated with dehydration, hormonal changes, and immune stress—all of which can increase urate levels.
- Illness: Severe illness, such as a heart attack, causes inflammation, dehydration, and tissue breakdown, which can rapidly raise urate levels.
- Surgery: Surgery typically involves physical stress, inflammation, and dehydration.
- Urate-Lowering Therapy: As blood urate levels drop, existing crystals begin to dissolve and shed, temporarily increasing inflammation.
- Chemotherapy: Chemotherapy causes rapid cell breakdown, releasing purines that are converted into large amounts of urate.
- Joints: Gout most often affects the big toe but can also involve fingers and larger joints, such as the knee, shoulder, elbow, and hip.
- Bursae: Gout can inflame bursae, which are small, fluid-filled sacs that cushion the space between bones and nearby soft tissue, such as muscles, tendons, and skin, reducing friction around joints.
- Tendon Sheaths: Gout may affect the protective sheaths around tendons in the hands and feet, leading to pain and stiffness.
- Kidneys: High urate levels can cause kidney stones and kidney damage.
The development of gout occurs in four stages.
Stage 1: High Uric Acid Levels Without Symptoms
Normal urate levels are usually below 6.8 milligrams per deciliter (mg/dL) and can differ between men and women. Levels of 8 mg/dL or higher are considered abnormally high, a condition known as hyperuricemia. In the first stage of gout, urate levels are elevated, but there are no symptoms. Urate may begin to accumulate and form crystals around joints—most commonly in the foot—but hyperuricemia alone is not enough to diagnose gout. While abnormally high urate levels can be the initial stage of gout for some people, many with increased urate levels never develop gout symptoms.
Stage 2: Acute Gout
In this stage, urate crystals enter the joint fluid and trigger an intense inflammatory response. This process draws in immune cells and releases chemicals that cause:
- Sudden pain, redness, and swelling
The first attack, or flare, is usually when a person first becomes aware that they have gout. It typically affects just one joint and often starts at night. The pain intensifies quickly and can be excruciating, especially when the joint is moved or touched.
- Fever
- Rapid heartbeat
- General feeling of being unwell
- Chills (rare)
If someone experiencing a gout flare develops a high fever (over 101 degrees Fahrenheit) or severe symptoms such as chills, weakness, vomiting, rash, or shortness of breath, they should seek medical attention immediately. These signs may indicate a joint infection or another serious condition.
Stage 3: Intercritical Gout
After an initial gout flare, most people enter a symptom-free period known as intercritical (or interval) gout. During this stage, attacks occur intermittently, sometimes within months and sometimes years apart. A significant number of people experience a second attack within one year of the first episode.
Stage 4: Chronic Gout
The final stage of gout, known as chronic gout or gouty arthritis, occurs when urate crystals form larger deposits called tophi. These nodules most commonly appear at joints such as the big toe or elbow, but can develop anywhere in the body, including cartilage, bones, and under the skin.
- Persistent Joint Pain: Pain may persist even between gout flares.
- General Aching: This can be a dull, persistent soreness or discomfort in the joints.
- Kidney Stones: In at least 15 percent of people with gout, urate crystals form stones in the kidneys.
- Joint Deformity and Reduced Mobility: Prolonged crystal buildup can damage cartilage and bone.
- Synovial Fluid Test: A synovial fluid test is the most accurate way to diagnose gout by examining joint fluid or a tophus sample for urate crystals using a polarized-light microscope. The fluid is collected by joint aspiration, during which fluid is withdrawn from a joint or a tophus with a needle.
- Blood and Urine Tests: Blood and urine tests measure uric acid levels in blood, which are normally 3.5 to 7.2 mg/dL for adult males or 2.6 to 6.0 mg/dL for adult females. These tests can support a gout diagnosis but should always be used alongside other tests, not alone.
- Imaging Tests: Doctors may use X-rays, ultrasound, or specialized CT scans to distinguish gout from injuries, detect joint damage, and identify urate deposits or tophi.
Stage 1: High Urate Levels Without Symptoms
Patients are usually advised to make lifestyle changes, but the condition itself is generally not treated with medication at this stage.
Stage 2: Acute Gout
Acute gout treatment focuses on reducing pain and inflammation during attacks and managing urate levels to prevent future flares.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs help reduce pain and swelling during a gout flare. Common options include ibuprofen (800 milligrams, taken three to four times daily) or indomethacin (25 to 50 milligrams, taken four times daily).
- Colchicine: Oral colchicine reduces inflammation caused by urate crystals and is most effective when taken early in a flare. Lower doses are better tolerated and can be combined with NSAIDs, while intravenous colchicine is avoided due to the serious risk of toxicity.
- Corticosteroids: Corticosteroids are used when NSAIDs cannot be taken or are not effective. Corticosteroids may be injected into affected joints for one or two joints, or taken orally, such as prednisone (30 to 40 milligrams daily, tapered over 10 to 14 days) for more widespread inflammation.
2. Future Recurrent Flare-Up Prevention
Stage 3: Intercritical Gout
Even without symptoms, urate continues to accumulate in the blood and joints during this stage, making it an important time to begin long-term treatment to prevent future attacks and complications.
- Uric Acid-Lowering Therapy: Uric acid-lowering therapy reduces gout attack frequency, prevents tophi, and lowers the risk of joint damage and other complications over time. Because starting therapy can trigger a gout flare, doctors often pair it with preventive medications, such as steroids, colchicine, or NSAIDs, to reduce this risk.
- Allopurinol: Allopurinol lowers uric acid by slowing the body’s production of it and is usually the first treatment prescribed. It is effective and affordable, but regular blood tests are needed to monitor kidney and liver function and to prevent side effects, such as rashes or changes in blood counts.
- Febuxostat: Febuxostat works similarly to allopurinol by lowering the body’s production of uric acid. It is typically reserved for patients with mild to moderate kidney disease or for those who can’t tolerate allopurinol. Regular blood tests are needed to monitor liver function and ensure the medication is being processed safely. A 2025 study involving more than 300 participants found that, in men with gout and low urine pH (below 6.2), adding urine alkalization to febuxostat therapy improved serum lipid profiles and decreased gout flares.
- Probenecid: Probenecid helps the kidneys remove more uric acid through the urine. It is used in people with normal kidney function whose kidneys do not eliminate uric acid efficiently. Probenecid helps the kidneys flush out more uric acid in the urine, increasing the risk of kidney stones, so good hydration is important. It is not recommended for people with kidney stones or gout-related kidney disease and is generally limited to those under 60.
- Pegloticase: Pegloticase helps the body break down uric acid so it can be more easily removed in the urine. It is typically used for people with severe gout who have not improved with standard treatments. Caution is advised in people with a history of cardiovascular disease.
Stage 4: Chronic Gout
At this stage, urate-lowering medications and lifestyle modifications should continue to be used to prevent flares and long-term complications.
- Sodium-Glucose Cotransporter-2 Inhibitors (SGLT2): A 2023 meta-analysis found that people with Type 2 diabetes who take SGLT2 inhibitors have about a one-third lower risk of developing gout. These medications may be a useful treatment option for people with diabetes who are at high risk of gout.
- Interleukin 1-Beta Inhibitors: Medications that block interleukin 1-beta inhibitors, such as anakinra, canakinumab, and rilonacept, target the inflammation directly and have shown benefit in treating acute gout flares. A 2023 systematic review found that canakinumab and rilonacept were more effective than comparators in relieving pain and reducing gout flares, while anakinra provided similar pain relief.
1. Self-Care Tips
During a gout flare, several strategies can help reduce pain and swelling. Cold therapy may help calm a flare; applying ice or a cold pack for 10 to 20 minutes at a time, with a cloth placed between the ice and the skin, can reduce swelling. Elevating the affected limb above heart level may further reduce swelling.
2. Diet and Certain Foods
Combining dietary changes with medication can improve treatment outcomes, particularly for people with severe gout. Although dietary changes don’t cure gout, they can reduce flares and help slow joint damage.
- Mediterranean Diet: The Mediterranean diet emphasizes fruits and vegetables, whole grains, beans, nuts, and seeds, olive oil, and limited red meat and sweets. While many types of seafood are restricted, people with gout can still eat salmon in moderation.
- DASH Diet: The Dietary Approaches to Stop Hypertension (DASH) diet is rich in fruits, vegetables, nuts, beans, and low-fat dairy, and low in red and processed meats and sugary drinks. A long-term study of about 44,400 men found that following a DASH-style diet lowered gout risk by 32 percent, while eating a typical Western diet increased risk by 42 percent.
Foods to emphasize include:
- Cherries: A 2019 systematic review found that people who regularly eat cherries or cherry products tend to have fewer gout flares and lower uric acid levels. An earlier study reported about a 35 percent reduction in gout attacks associated with cherry intake, with risk reduced by 75 percent when cherries were combined with the urate-lowering medication allopurinol.
- Other Beneficial Foods: Spinach, celery, eggplant, tomato, green beans, asparagus, raisins, black currants, banana, apricots, orange, and apples, as well as complex carbohydrates such as beans, brown rice, nuts, oatmeal, and starchy vegetables.
Foods to limit or avoid include organ meats, such as brains, liver, and sweetbreads, as well as kidneys, broths, gravies, and oily fish, including sardines and anchovies.
3. Hydration
Drinking plenty of water is helpful for managing gout, especially if kidney stones are present, as water can help the body remove excess urate. Limiting beverages sweetened with corn syrup (glucose-fructose), fruit juices such as orange or apple juice, and fruit juice concentrates may also help reduce gout risk.
4. Dietary Supplements
Some dietary supplements may support gout management, although they should be used cautiously and in consultation with a health care provider.
- Vitamin C: By potentially slowing purine metabolism, vitamin C can indirectly reduce urate production. A 2011 meta-analysis of 13 studies found that taking about 500 milligrams of vitamin C daily for about one month slightly lowered blood uric acid levels. However, high doses of vitamin C may increase the risk of kidney stones.
- B Vitamins: A 2018 study found that B-vitamin supplements, especially folate (vitamin B9) and vitamin B12, were associated with lower urate levels in men. However, the same benefit was not clearly seen in women.
- Omega-3 Fatty Acids: People with higher levels of omega-3 fatty acids have fewer gout attacks. This suggests that regularly taking omega-3 fish oil, which has anti-inflammatory effects, may help prevent gout flares—especially when starting uric acid-lowering treatment, but more research is required.
5. Regular Moderate-Intensity Exercise
People with gout who remain physically active tend to have fewer flares each year, lower inflammation levels, and less pain than those who are inactive. Experts recommend aiming for at least 30 minutes of physical activity each day. However, exercises should be carefully chosen to avoid worsening joint pain or placing excessive strain on affected joints. Between gout flares, people can safely engage in aerobic and strengthening exercises.
6. Warm Ginger Compress Therapy
Warm ginger compress therapy involves placing a warm cloth soaked in ginger extract on the painful joint. This noninvasive approach may help manage symptoms of gouty arthritis. A 2023 study involving 30 gout patients found that combining warm ginger compresses and static stretching for 15 to 20 minutes, six times over two weeks, significantly reduced joint pain compared with a control group.
- Coffee Intake: A 2022 study found that drinking coffee was associated with a lower risk of gout, even when urate levels were taken into account. Researchers noted that the components in coffee may offer new insights into gout prevention.
- Illness Management: Because many medical conditions increase gout risk, prompt and ongoing management after diagnosis is important.
1. Combined Comorbidities and Complications
Many people with gout often experience overlapping comorbidities and complications, including:
- Mental health issues such as depression and anxiety
- Osteoarthritis and joint damage
- Underactive thyroid
- Erectile dysfunction
2. Comorbidities
Other common comorbidities include:
- High blood pressure
- Obesity
- Diabetes
- High cholesterol
- Congestive heart failure
- Heart attack
- Chronic lung disease
- Anemia
- Psoriasis
3. Complications
Some gout-related complications can be serious and long-lasting, including:
- Permanent joint damage
- Increased risk of cardiovascular diseases
- Narrowing of the arteries
- Kidney stones and kidney disease
- Metabolic syndrome
- Higher risk of certain cancers, such as prostate cancer
- Bone loss
- Joint deformity
- Panniculitis (inflammation of the layer of fat beneath the skin)
- Conjunctivitis (pink eye)
- Chronic arthritis
- Recurrent flares
- Tophaceous deposits (tophi)