Measles: A Complex Challenge in the Face of Global Resurgence
Measles, also called rubeola, primarily spreads as an airborne particle, posing a significant risk of transmission. However, its ability to survive on surfaces for over two hours makes it even more concerning, extending its infectivity window. A person with measles can potentially transmit the virus to 90 percent of the people with whom they come in contact.
Phases and Potential Complications
Measles infection progresses through three distinct phases:
- Incubation phase: This initial phase lasts approximately 10 to 14 days, with no symptoms present. The virus silently replicates within the body.
- Prodromal phase: Following the incubation period, the prodromal phase emerges, lasting two to four days. Symptoms such as high fever, cough, runny nose, and small white spots (Koplik spots) on the inside of the cheeks become evident.
- Rash phase: The rash phase is a hallmark of measles, typically lasting 2-4 days. It begins on the face and subsequently spreads downward over the body.
Measles can be quite taxing on the infected person. In the United States, approximately 1 in 4 measles patients require hospitalization, and the infection claims the lives of about one to three individuals per 1,000 cases. Moreover, measles can lead to severe complications.
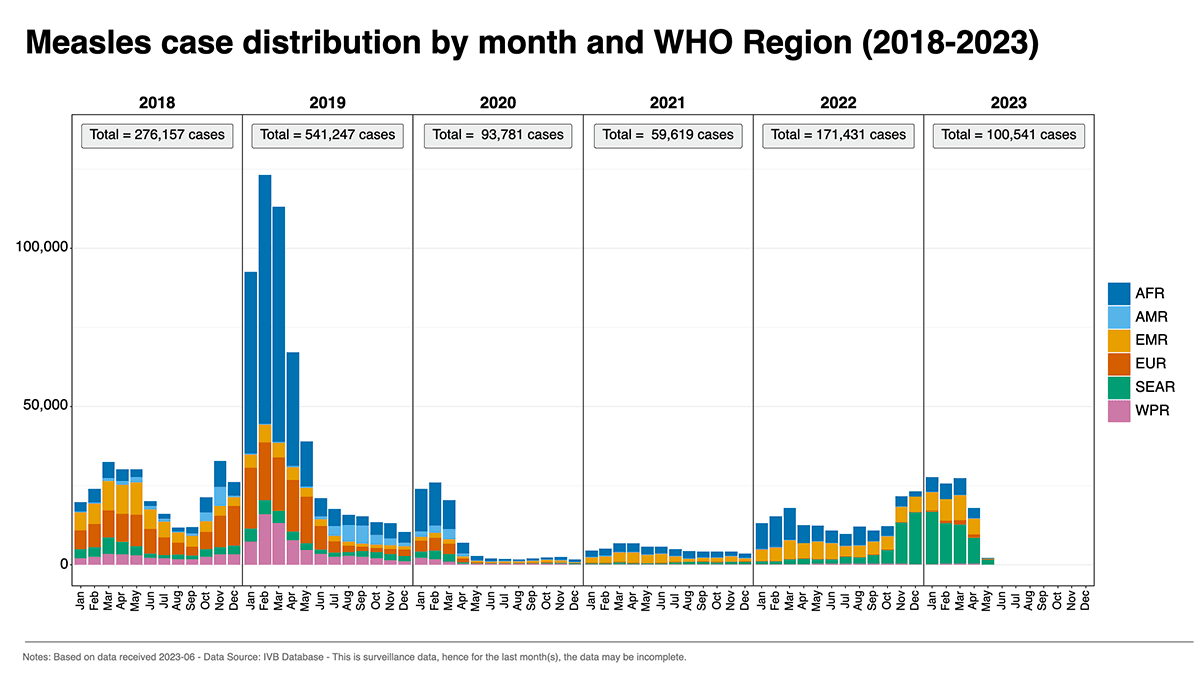
The Impact of the Pandemic on Vaccination Efforts
In late 2021, the WHO issued a notice warning of the pandemic’s threat to the progress made against measles worldwide. The global initiative was meant to reduce measles to a minimum worldwide, but in 2022, approximately 40 million vulnerable children remained susceptible to measles because they missed a vaccine dose.
Vaccination Campaigns Can’t Eliminate Measles
Measles vaccines are primarily categorized into two types:
- Measles-Mumps-Rubella (MMR) vaccine: The MMR vaccine is a combination vaccine that protects against measles, mumps, and rubella. Administered in two doses, typically at 12 to 15 months and 4 to 6 years of age, it contains weakened live viruses for each disease, providing long-lasting immunity against measles.
- Measles-Mumps-Rubella-Varicella (MMRV) vaccine: Another combination vaccine, this protects against measles, mumps, rubella, and varicella (chickenpox). Like MMR, it contains weakened live viruses and is commonly used as an alternative to separate MMR and varicella vaccines for children aged 12 months to 12 years. It is typically administered in two doses.
Breakthrough cases, where vaccinated individuals contract the virus, can occur in areas with low vaccination rates (less than 10 percent of cases) and even in areas with high rates (more than 10 percent of cases). Such cases can result from primary vaccination failure (complete rejection of the vaccine by the body) or secondary vaccination failure (waning immunity).
Breakthrough Infections: Measles Outbreaks After Vaccination
Studies on measles outbreaks have provided mixed results, with evidence demonstrating both the vaccine’s effectiveness in preventing spread and instances of virus acquisition among vaccinated individuals.
- Vaccine failure: While the measles vaccine is highly effective, it is not 100 percent foolproof. In a small percentage of individuals, the vaccine may not provide complete immunity or may wane over time. This can leave the person susceptible to infection if they come into contact with the measles virus.
- Improper timing or dosage: The effectiveness of the measles vaccine depends on factors like timing. Following the recommended two-dose schedule is vital for optimal protection. Incomplete vaccination or delays between doses increase the risk of breakthrough infections.
- Strain mismatches: The measles virus can vary in strains across regions and time, potentially leading to breakthrough infections if a vaccinated individual encounters a different strain than the one targeted by the vaccine. However, the vaccine offers a certain degree of cross-protection against various strains.
- Immune system factors: Underlying health conditions or certain medications that weaken the immune system can increase susceptibility to breakthrough infections. Age also influences immune response, with infants and young children exhibiting a less robust response to the vaccine.
Addressing Immune System Factors for Measles Prevention
The impact of immune system factors on public health requires serious consideration amid the rising measles cases in the past 10 years. We need to look at the population’s overall health conditions. People tend to blame the surging of viral pathogens on poor sanitation conditions, failure of vaccination campaigns or infection controls, and international travel.