This is what most women don’t know about hormone replacement therapy (HRT): Timing matters more than age. The key isn’t whether you’re 45 or 55 when you start HRT; it’s when you start relative to your menopause transition.
This concept, called the “therapeutic window” or “timing hypothesis,” accounts for nearly all of the modern controversy surrounding hormones. The wrong therapy, given to the wrong patients, at the wrong time, created decades of confusion.
‘Everything Feels Like It’s Slipping’
A few months ago, Laura (not her real name), 49, walked into my office with that mixture of hesitation and hope that is so common in midlife patients.
She had always been proud of her resilience. She ate well, exercised consistently, managed stress better than most, and had built a solid career that required sharp thinking and emotional steadiness.
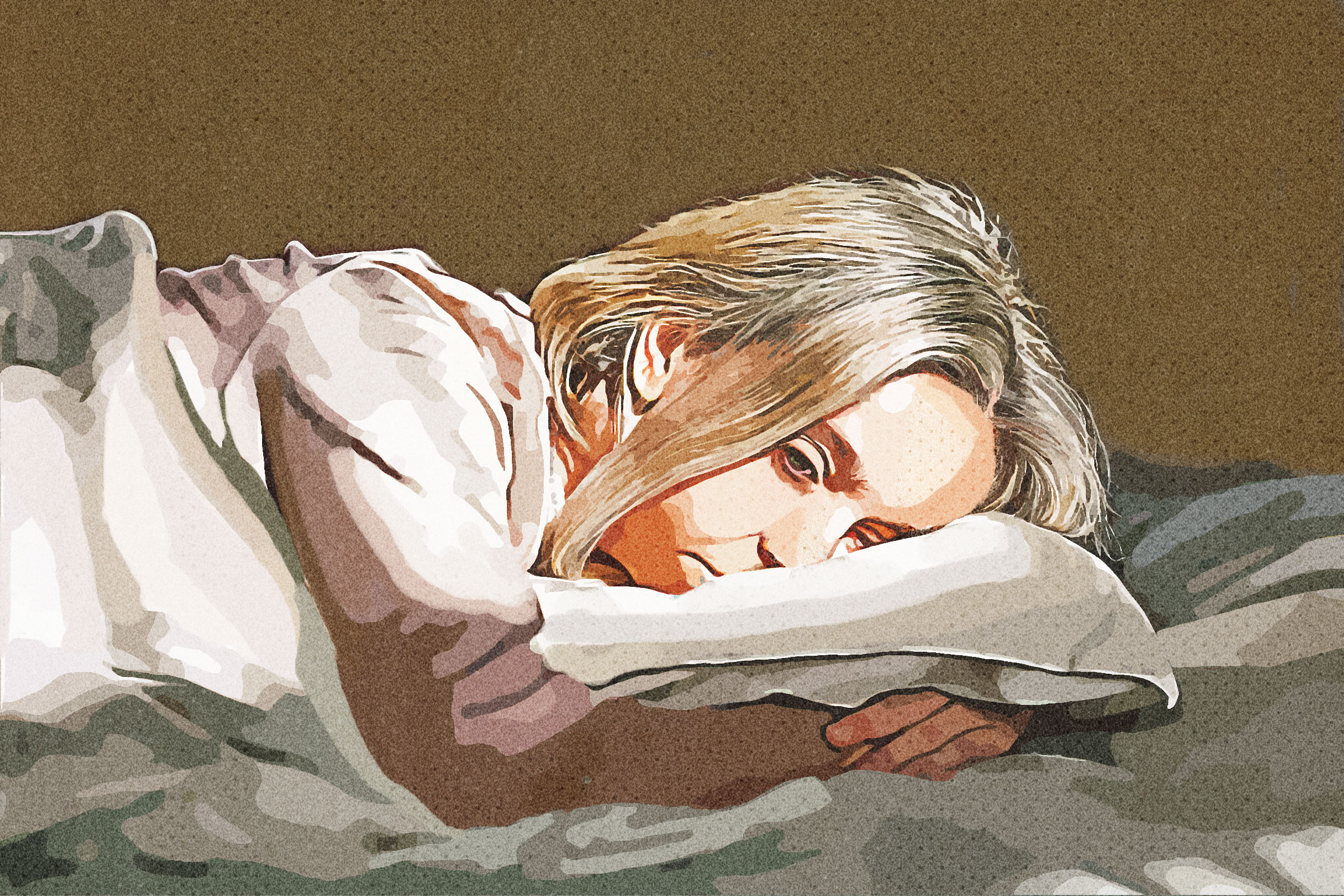
She began describing the symptoms she had told herself weren’t important: the hot flashes that woke her at 2 a.m., the sudden waves of anxiety that seemed to come from nowhere, the irritability that left her apologizing to her children, and the bone-deep fatigue that followed her through the day like a shadow.
However, then she said, “Recently, everything feels like it’s slipping.” Not falling apart, but slipping—quietly and subtly— in ways she couldn’t quite explain. And the symptom that frightened her most was the one she didn’t know how to articulate: “I can’t think clearly. I feel like there’s cotton where my brain used to be.”
I nodded, because I have heard that sentence—in one form or another—from hundreds of women. Brain fog. Cognitive drag. Lost sharpness. Mental fatigue. Women describe it in different ways, but the essence is always the same: a sense of no longer recognizing the mind they once trusted.
I asked Laura to tell me what had changed, not in her bloodwork or biology, but in her sense of self. How had she changed at home? At work? In her marriage? In her friendships? In her own quiet moments?
She hesitated, then the truth came out in waves—not dramatic, not exaggerated, just honest.
“I avoid social events now. I worry I’ll forget someone’s name.”
“I wake up with my heart pounding and I don’t know why.”
“I’m not depressed, but I don’t feel like myself.”
“I’m scared I’m losing something I won’t get back.”
This is what menopause actually looks like. Not just hot flashes and missed periods, but changes to identity, relationships, confidence, sleep, meaning, and the invisible threads that hold a woman’s daily life together.
Estrogen Is More Than a Reproductive Hormone
Estrogen is not simply a reproductive hormone—it is one of the brain’s most influential molecules.
It regulates serotonin (mood), dopamine (motivation), and acetylcholine (memory). It influences dozens of pathways affecting everything from anxiety to emotional stability. When estrogen drops suddenly, your brain recalibrates—sometimes smoothly, sometimes turbulently.
The turbulence isn’t a psychological weakness. It’s neurochemistry in transition.
Understanding this was profoundly relieving for Laura. And it should be for every woman navigating this transition.
‘Is Hormone Therapy Right for Me?’
At the end of her story, she took a deep breath and asked the question she had been holding back: “Is hormone therapy right for me?”
She asked it quietly, as though afraid the question itself was dangerous. That fear didn’t come from her. It came from two decades of cultural messaging that made women regard hormone therapy like a gamble rather than a medical option. Even now, with new Food and Drug Administration (FDA) guidance and a clarified scientific understanding, many women still carry the echo of old headlines inside their bodies.
Many women are treated by doctors who graduated during the height of anti-HRT fear and who do not feel equipped to guide patients through the nuances—timing, formulation, dosage, route of administration, and risks—even when they are willing to prescribe hormones.
After listening to Laura’s story, we talked about the science.
Hormone therapy is most effective and safest when started within a specific window of time.
When estrogen is introduced around the beginning of menopause, it behaves like a partner to the body, stabilizing blood vessels, supporting brain function, protecting bone, and calming the nervous system.
However, when introduced 10 or more years after menopause, the body’s terrain has changed—blood vessels are stiffer, inflammatory pathways more active—and the therapy behaves differently.
Nearly all the modern controversy about hormones stems from using HRT in the wrong patients at the wrong stage of life.
Laura’s shoulders relaxed. “Why didn’t anyone explain it this way?” she asked. It’s a fair question—and one that deserves an honest answer.
When HRT Is Appropriate–and When It Isn’t
Once we had walked through the science and her symptoms, I said to Laura that hormone therapy is not a universal solution.
First of all, some women shouldn’t use it—those with certain cancers, untreated cardiovascular conditions, or specific medical histories.
Then, some are better served by nonhormonal treatments such as selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, or gabapentin for menopausal hot flashes and night sweats, as well as newly approved medications such as elinzanetant, which the FDA recently cleared as a nonhormonal therapy for hot flashes.
However, for the right woman—particularly one in her late 40s or early 50s—hormone therapy can be life-changing. It can restore sleep, ease anxiety, support cognition, calm vasomotor storms, preserve bone, improve metabolic health, and reawaken a sense of vitality that menopause often dims too early.
I told Laura something that often surprises women: “Hormone therapy isn’t a decision you make all at once. It’s a conversation you enter. You don’t need to commit to something permanent. You simply need to decide whether we should take a step forward together.”
The first step is always the same: understanding yourself. What are you losing? What do you want back? What worries you? What matters most? What do you hope this next chapter of life will be? Only once those questions are answered can we ask the medical ones.
Laura was quiet as she absorbed this.
Finally, she said, “I thought menopause meant I had to suffer. I didn’t realize I had options.”
That sentence captures the experience of millions of women.
1 Month Later
Laura began a low-dose transdermal estradiol patch, which delivers estrogen through the skin, paired with micronized progesterone, a hormone that protects the uterine lining. Within a month, she said, “The fog is lifting.” Not completely—but noticeably enough that her children said she seemed more like herself.
That is the quiet power of menopause medicine—not youth restored, but selfhood returned.
Menopause is not an ending. It is a crossing. And with the proper support, it can be a crossing into clarity, energy, wisdom, and confidence.
In the process, Laura realized that her suffering is not trivial, that her well-being is not negotiable, and that she has the right to reclaim a life that feels like her own.