At 26, Dani Homer could barely get through a day. She slept through weekends, ate little, and felt as if her limbs were made of lead. Yet every doctor she saw told her that she was fine.
“I must have heard my labs were normal a couple dozen times,” she said.
Later, a more comprehensive thyroid panel revealed Hashimoto’s disease, an autoimmune condition that earlier lab tests had missed. Although disease was present, the tests were examining the wrong places, missing the diagnosis.
Across the country, many patients leave appointments with normal results but no clarity about why they feel unwell. Normal on paper doesn’t always match what the body is trying to say, and that gap between the numbers and the lived experience is often where the real problem lies.
Clinicians want to help, but the system rewards speed over pattern recognition. That leaves patients with a task most were never taught: knowing their own numbers well enough to be able to recognize when something deserves a closer look. When you can spot meaningful shifts in your lab results, you are far better equipped to push for answers and avoid treatment you don’t need.
Why ‘Normal’ Isn’t Always Normal
When a doctor says your labs are normal, it sounds like a clean bill of health. Often, it is. However, normal in laboratory medicine lingo means within a reference range, not necessarily optimal levels or the levels at which you feel great. Normal simply indicates how you compare with everyone else.
Here’s how ranges are set: Labs collect results from people they consider to be healthy, remove the outliers, and label the middle 95 percent as normal.
“That is statistics, not physiology,” Brad Rachman, a functional medicine physician and former director of medical science at Genova Diagnostics, told The Epoch Times. “In the lab world, it means two standard deviations from the mean—a calculation dating to 1930s agricultural studies.”
Each lab defines “healthy” differently, and there’s no national standard. Federal rules ensure accuracy but not uniformity, so a result that appears accurate in one lab may be flagged as incorrect elsewhere.
Differing definitions of “healthy” matter. Harvard Medical School and Stanford University researchers found that when “healthy” was defined differently—for instance, excluding people with chronic disease, focusing on young adults, or using only those who rated their health as excellent—as many as one in four people switched from normal to abnormal for the same test.
There is a deeper problem. As the population grows heavier and sicker, averages drift upward. Higher blood sugar or cholesterol levels become more common, and therefore more normal. Many lab ranges haven’t been meaningfully updated in decades, according to Rachman, meaning that what looks fine today might have been a red flag a generation ago.
Technology adds one more wrinkle. Different labs use different equipment and calibration methods, Alan Wu, chief of clinical chemistry and toxicology at the University of California–San Francisco, told The Epoch Times, which is why every report lists its own reference range.
The Case for Trends
When what is called normal can vary from lab to lab, what matters more than a single result is the direction in which your lab trends are moving.
“Blood biomarker trends carry more weight than a single in-range result,” Dr. Ionela Hubbard, a preventive medicine professor at Loma Linda University, told The Epoch Times in an email. Watching how values move over time, according to her, helps distinguish true physiological changes from the normal day-to-day fluctuations that come with stress, sleep, medications, or time of day.
Each person’s body runs on its own rhythm. Most people’s blood counts hover around a personal set point that is as distinctive as a fingerprint, a 2024 study published in Nature found, and those values can stay stable for decades.
A fasting glucose level of 95 might be considered healthy for one person, but it signals an early change for someone whose usual level is 80.
“Knowing where a patient’s numbers were 10 years ago tells me far more than any single result today,” Dr. Aaron Erez, an internist focused on metabolic and preventive health, told The Epoch Times.
Trends also reveal relationships within the body. A slow climb in blood sugar, a steady drop in vitamin D, a gradual rise in inflammation: These patterns show where the body is headed, not just where it stands. The thyroid affects metabolism, which in turn shapes cholesterol levels and mood.
“The average clinician has 12 minutes [with a patient],” Rachman said. “They’re looking at a snapshot, not a movie.”
When results are read in isolation, systemic connections can be lost. Functional and integrative physicians often track labs, connecting the dots across years, but anyone can do the same. You can download your results, save them in a folder or spreadsheet, and note their direction over time.
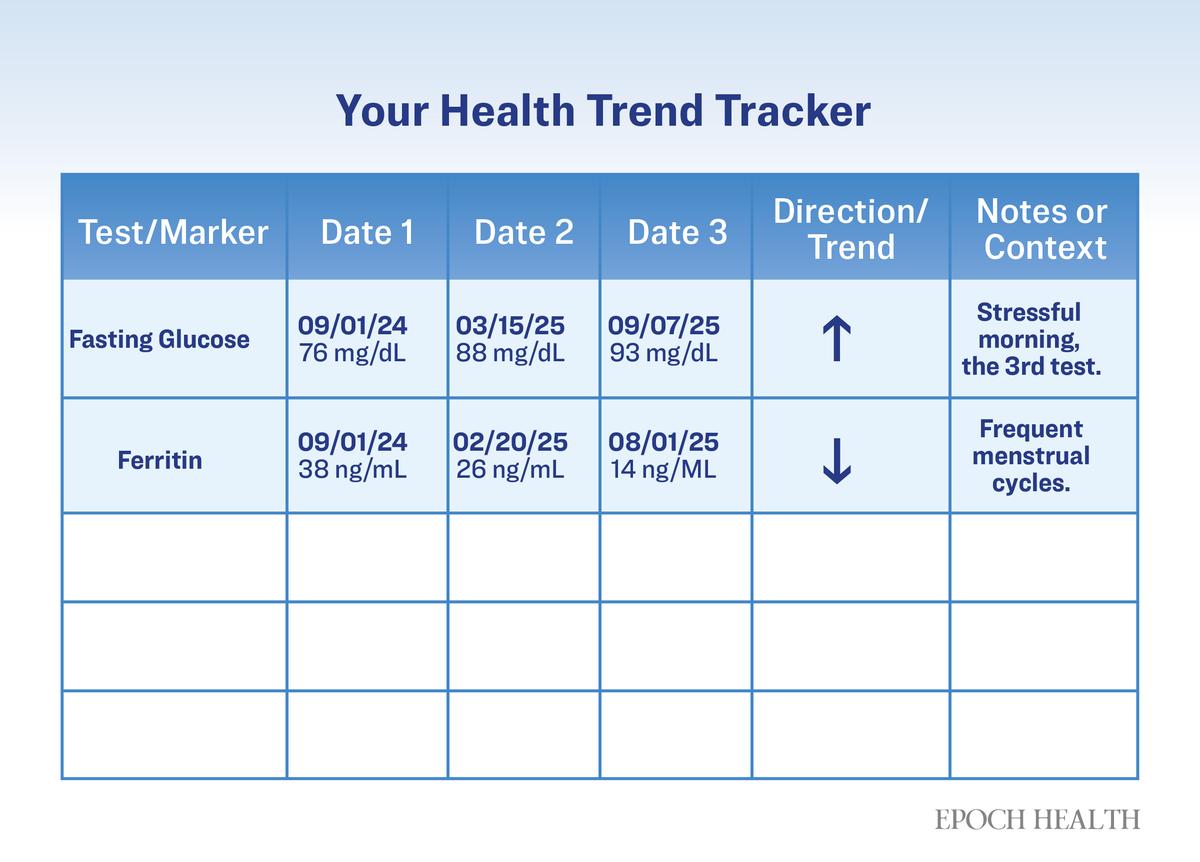
How to Track Your Labs
If your online health portal doesn’t track and graph your labs, you can do it yourself with a simple spreadsheet or notebook. The goal isn’t to find meaning in every number, but to track direction over time.
- Choose What Matters Most: Start with five to 10 markers that you and your clinician watch regularly. These may include glucose, hemoglobin A1c, iron and ferritin, vitamin D, thyroid hormones, C-reactive protein, or cholesterol.
- Record Results by Date: Add new entries in the same lab’s units and note the testing location if it changes.
- Mark the Movement: Circle or color-code gradual rises or drops instead of focusing on single spikes.
- Add Brief Context: A note such as “started new supplement,” “training for race,” or “poor sleep this month” helps explain shifts that aren’t disease-related.
- Review Before Appointments: Patterns can prompt better questions about what’s improving, what’s slipping, and why.
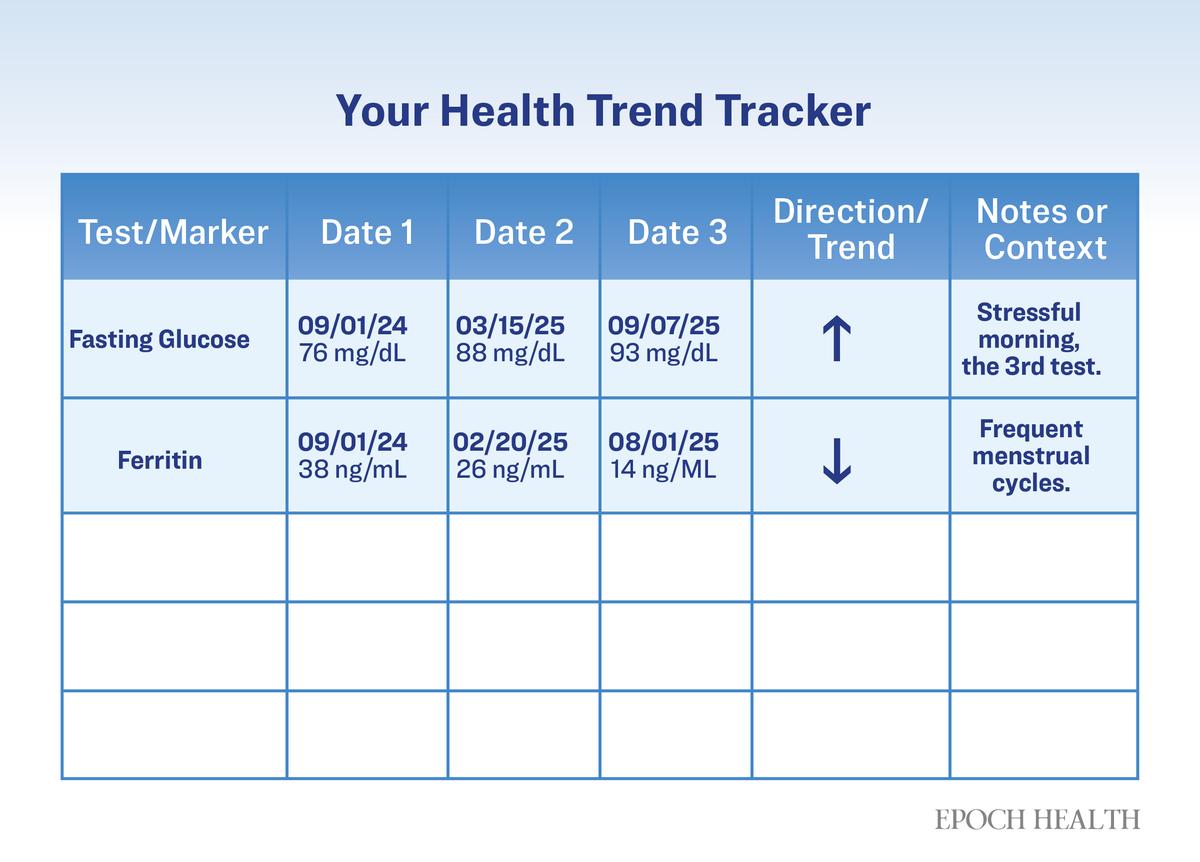
A simple tracker can reveal rising or falling patterns that a single lab result may miss.
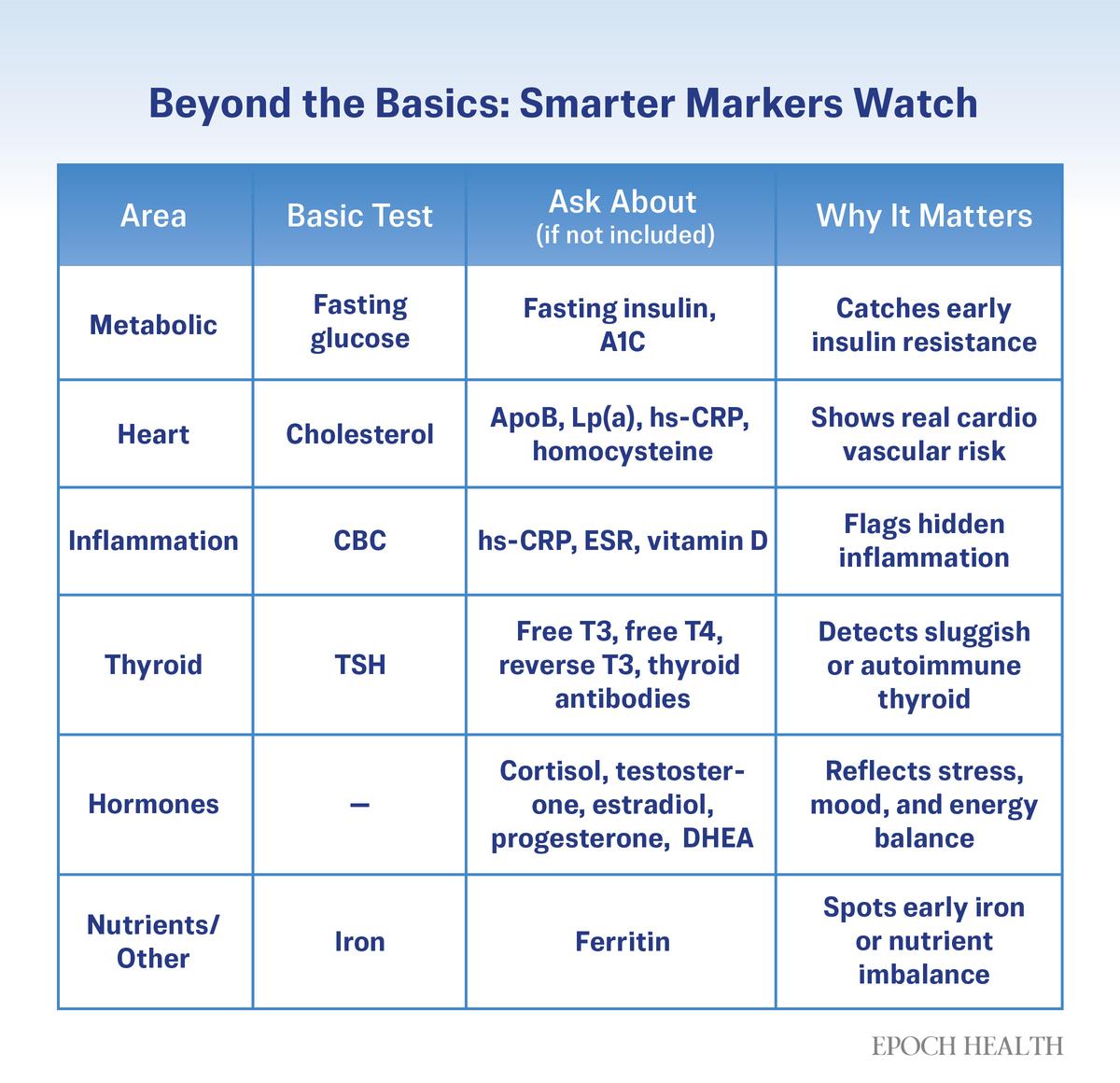
When Standard Panels Stop Too Soon
Even the clearest trend can be misleading when key markers are never checked. Routine bloodwork can miss the bigger picture. A cholesterol test may show total cholesterol—low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides—but overlook markers such as low-density lipoprotein particle size or apolipoprotein B that better capture heart disease risk. Iron can look fine, too, while ferritin—the body’s iron storehouse—is quietly running low.
If doctors know that more specific tests exist, why aren’t they ordering them? Most follow preset orders built for efficiency, insurance coverage, and billing codes.
Many labs also use automated “test cascades,” in which follow-up tests are run only if the initial result exceeds a certain threshold. It’s efficient, but it can halt the search too soon.
Hubbard said this is one area in which patients and clinicians often need a broader view. When symptoms persist or patterns shift, she said, expanding the panel to look at related markers can reveal early dysfunction long before values are marked as abnormal. Consider thyroid testing. A thyroid-stimulating hormone level may look normal yet hover near the edge of concern. Because it hasn’t triggered the lab’s cutoff, deeper tests such as free T3, free T4, and thyroid antibodies are never run, and early autoimmune disease can be missed.
“Most lab orders aren’t curiosity-based,” Rachman said. “The real art is asking why that value keeps creeping up, why the pattern doesn’t fit, why the patient still feels unwell.” However, when curiosity turns into fixation, the search for answers can create its own problems.
When Paying Attention Becomes Overdoing It
Awareness can empower, but it can also overwhelm. Once people start learning about lab markers and optimal ranges, it’s easy to chase every number.
“It becomes shotgunning,” Rachman said. “They’re looking for answers but creating noise.”
Research backs his theory up. A 2025 study published in Archives of Pathology & Laboratory Medicine found that nearly one in four Americans received lab tests more often than guidelines recommend. These screenings rarely changed treatment but often led to more testing and anxiety. Other research associates excessive blood draws with tangible harm, from anemia to needless procedures.
Normal day-to-day fluctuations—driven by stress, sleep, or even the time of day—can look alarming out of context. Reacting to every blip fuels more worry and more testing.
So how do you know when to stop? The key is pattern and persistence, according to Rachman. Test deliberately, not reflexively: when symptoms linger, when a clear trend appears in your baseline numbers, or when a result doesn’t fit how you feel.
“Knowing when to stop is as important as knowing when to start,” Rachman said.
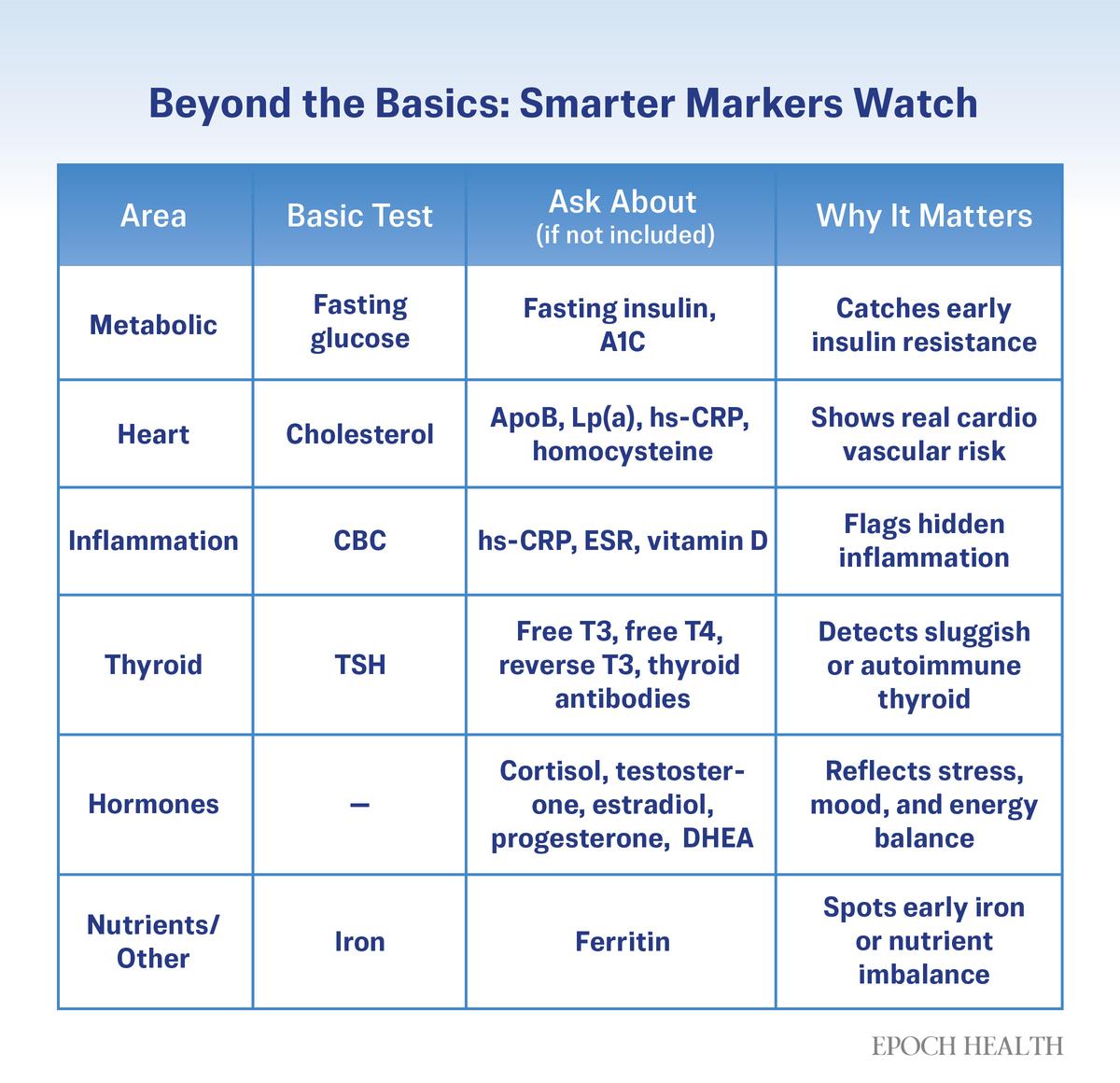
Supplemental markers can clarify risk and detect health issues that may not be reflected in standard tests.
Making Sense of Your Results
Seeing your test results can be both reassuring and unnerving. However, what matters most isn’t the color codes or arrows; rather, it’s the context: what’s typical for you, what’s changing, and what might warrant another look. Here’s how to start making sense of your results:
- Watch Your Baseline and Trend: Most patient portals now automatically graph results, showing how values shift over time. If yours doesn’t, keeping a simple log or spreadsheet can help reveal meaningful trends.
- Try to Use the Same Lab Network Each Time: Even when your doctor orders the same test, results can vary depending on where the sample is processed. Different laboratories use different machines and methods, which can result in slight variations in the numbers. Keeping your tests within the same lab network such as Quest or Labcorp makes tracking trends more reliable. If your provider switches labs, make a note of it so you can interpret future results.
- Don’t Panic Over an Unusually High or Low Result: Bodies fluctuate. One high or low reading rarely means much on its own.
- Know What Matters: Some tests measure critical electrolytes and organ function: for example, sodium, potassium, creatinine, or liver enzymes. Even small shifts in these numbers can be significant. But vitamin D, cholesterol, and ferritin have broader optimal zones and the significance of shifts in these levels depends more on your overall picture and symptoms.
- Ask What’s Optimal, Not Just Normal: Normal reflects averages, not ideals. Many people feel better with vitamin D levels closer to 50 nanograms per milliliter, even though 30 nanograms per milliliter is considered normal.
When to Ask for a 2nd Look
Even when you understand the numbers, the ranges, and your own trends, you may still feel that something isn’t right. That’s when a second look helps. Ask for another screening when:
- Labs Look Fine on Paper, but You Don’t Feel Fine: Lingering fatigue, brain fog, or mood changes can signal problems that routine panels miss. Of course, not every symptom points to a hidden disorder; poor sleep, stress, or even constant screen time can take a toll that no blood test will show. Still, when symptoms persist, Rachman encourages patients to stay curious. “If you don’t ask the right questions, you won’t get the right answers,” he said. “Keep asking why—why that number keeps creeping up, why you still don’t feel well.”
- Your Numbers Are Drifting: A steady rise in blood sugar or liver enzymes, or a slow decline in ferritin or vitamin D, can hint at an imbalance long before results turn red.
- The Picture Seems Incomplete: Some tests stop too soon, such as thyroid panels that omit antibodies or cholesterol tests without apolipoprotein B. If a result seems borderline, you can ask whether a cascade test applies or whether there’s a related marker that would give a clearer picture.
- Something Else Has Changed: New medications, supplements, or diet shifts can alter results. Tell your doctor.
- You Want Another Perspective: If you still feel that something is off, look for a clinician who connects the dots: an internist, endocrinologist, or integrative physician trained to see how systems involving hormones, metabolism, and mood interact. According to Hubbard, a broader lens can reveal relationships that routine panels miss.
If access is an obstacle, certified direct-to-consumer services such as Quest Diagnostics, SiPhox Health, or Everlywell can help fill some gaps. They are not a replacement for medical care, but they can open conversations that might otherwise never happen.
Finding Meaning in the Numbers
“There are three people in the room—you, your doctor, and the wise one inside you,” Rachman said. When that inner sense is dismissed, patients often lose trust. Yet it’s often the body’s first diagnostic clue.
For Homer, the hardest part wasn’t the illness; it was being told that nothing was wrong. Each normal result deepened her doubt until she began to question her own experience.
After finally being diagnosed with Hashimoto’s, she learned to track her thyroid markers—thyroid-stimulating hormone, free T4, and antibodies—alongside how she felt day to day. With diet and lifestyle changes, she brought most symptoms into remission and reduced her antibodies by 90 percent.
“Trust your body,” she said. “You know it better than anyone else. It’s not all in your head.”
What’s Next: When your story and your labs don’t match, your next step might be a second opinion and a pause. Our next article will explore when to seek another set of eyes, how often second opinions change treatment, and why slowing down can spare months of incorrect care.