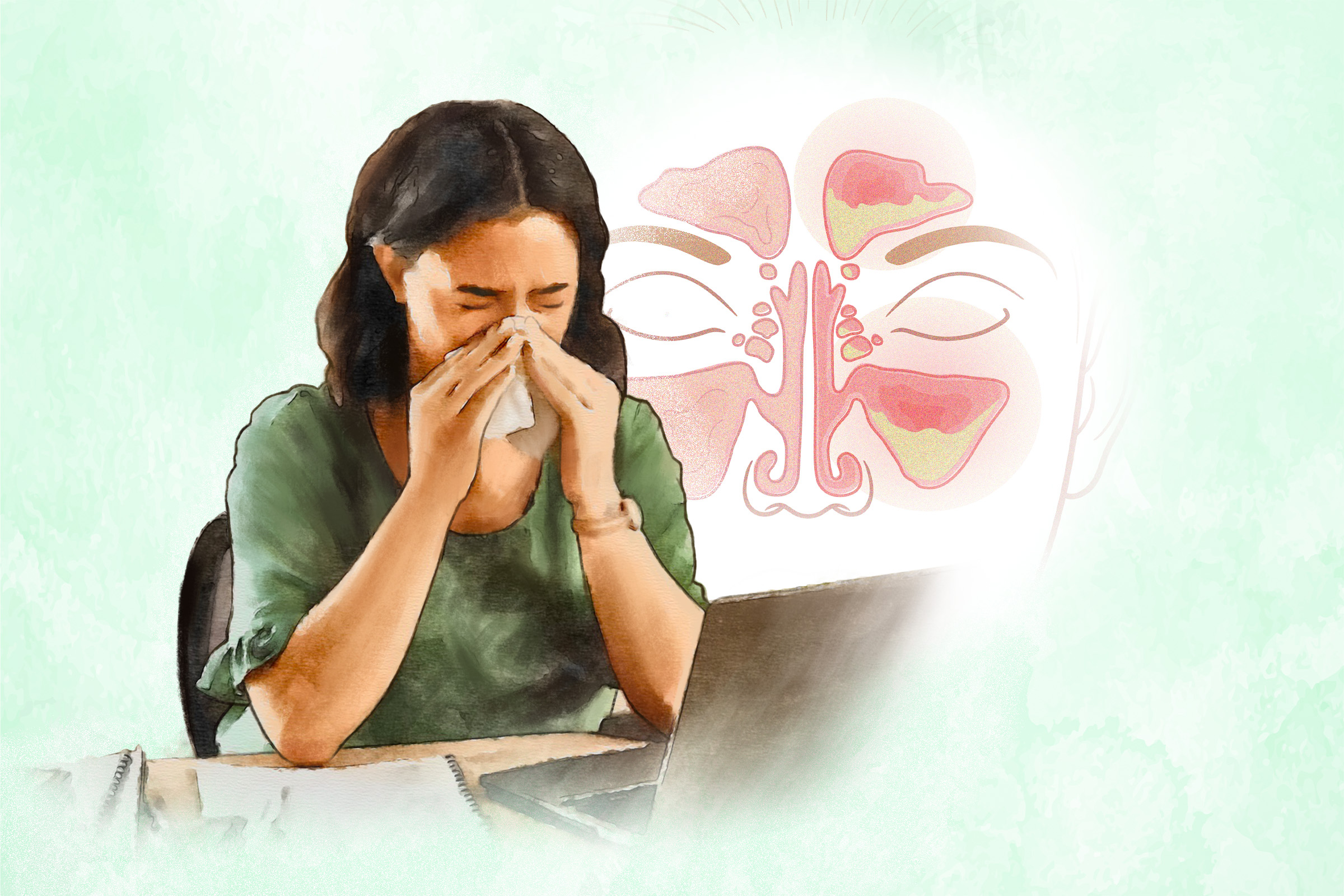
- Ethmoid sinuses are located near the top of the nose, around the bridge. They are present at birth.
- Maxillary sinuses are found next to the lower nose and over the cheekbones. They are also present at birth.
- Frontal sinuses are in the forehead, just above the eyebrows. They develop in mid-childhood.
- Sphenoid sinuses are positioned behind the nose. They develop in adolescence.
A sinus infection can be classified based on which pair of sinuses it affects. It can also be classified based on its duration and underlying cause.
Duration
Sinus infections can be classified by their duration. These categories include the following:
- Acute sinusitis is a short-term inflammation of the sinuses, typically lasting less than four weeks with full resolution. The condition in healthy individuals is usually caused by viruses. Sometimes, a bacterial infection can develop afterward. Sinus infections acquired in hospitals are often bacterial. Symptoms such as nasal discharge (typically thicker than what comes from a runny nose), nasal congestion, and facial pain usually improve within 10 days but can persist for a few weeks. In some cases, symptoms may temporarily improve before worsening again.
- Subacute sinusitis is a continuation of acute sinusitis, characterized by symptoms lasting between four and 12 weeks.
- Chronic sinusitis is a long-term inflammation of the sinuses lasting 12 weeks or more. While symptoms can persist, many people recover with proper treatment. Some subtypes of chronic sinusitis include chronic sinusitis without nasal polyps (soft, noncancerous growths that develop in the lining of the nose and sinuses), chronic sinusitis with nasal polyps, and allergic fungal sinusitis, which takes place in people with normal immune systems. It causes a thick, mass-like buildup in the sinuses, leading to long-lasting sinus symptoms.
- Recurrent sinusitis involves four or more acute episodes lasting at least 10 days each within a single year. The condition resolves between episodes but recurs multiple times annually.
Cause
Sinus infections can also be classified by their cause. These categories include the following:
- Viral sinusitis is a common condition caused by a viral infection. It often follows upper respiratory infections, such as a cold or flu. Viral sinusitis is self-limiting, generally resolving within a week without specific medical intervention.
- Bacterial sinusitis is caused by bacteria, often following a viral illness. Most cases resolve within two weeks without recurring symptoms.
- Allergic sinusitis occurs when allergens such as pollen or dust inflame the sinus membranes, often leading to a sinus infection. In addition to typical sinus symptoms, allergies can cause itching in the eyes, nose, or throat.
- Fungal sinusitis is categorized as noninvasive or invasive based on the extent of the fungal infection and its impact on the sinuses. Noninvasive types are confined to the nose and sinus regions, including fungal ball, saprophytic fungal sinusitis, and allergic fungal rhinosinusitis. Invasive types can spread to the eyes and brain and are more common in people with weakened immune systems.
- Purulent (pus-related) drainage: green or yellow nasal discharge
- Facial or dental pain: aching, fullness, or pressure-like pain
- Nasal obstruction: difficulty breathing through one or both nasal passages that often leads to mouth breathing and possibly snoring at night
Other signs and symptoms may include:
- Pain, swelling, and tenderness around the cheeks, eyes, or forehead.
- Runny nose.
- Reduced sense of smell (hyposmia).
- Fever: Although fever is present in around half of sinusitis cases, it can still be an important sign of how severe the condition is.
- Postnasal drip (mucus draining from the nose into the back of the throat).
- Headache.
- Bad breath (halitosis).
- Cough that often worsens at night.
- Pressure sensation in the ears.
- Fatigue.
- Ear pain.
- Sore throat.
Sinusitis symptoms and signs in young children may include:
- Irritability
- Difficulty eating
- Breathing through the mouth
- Swelling around eyes
- Nausea and poor appetite
- Cold or respiratory illness that improves but then worsens again
- High fever with dark nasal discharge lasting at least three days
- Nasal discharge that lasts over 10 days without improvement, with or without a cough
Often, where a person experiences pain, discomfort, or other symptoms in his or her face will indicate which sinus is infected. Acute and chronic sinusitis symptoms are similar, but chronic sinusitis symptoms are generally milder.
Environmental Factors
- Viruses: Acute sinusitis is usually caused by viruses, including rhinovirus (which causes common colds), adenovirus, influenza (flu) virus, and parainfluenza virus (which causes colds, bronchitis, and pneumonia).
- Bacteria: Bacteria can also cause sinus infections, with the most common culprits being Streptococcus pneumoniae (38 percent), Haemophilus influenzae (36 percent), and Moraxella catarrhalis (16 percent).
- Fungi: Fungal infections can sometimes cause sinus infections, but this is very rare and usually occurs in people with weakened immune systems, including those with uncontrolled diabetes, HIV, or certain autoimmune diseases or who are undergoing cancer treatment or organ transplant. The fungi that can cause these infections are typically Mucor, Rhizopus, Rhizomucor, and Aspergillus.
- Smoke, chemicals, or fumes: Tobacco smoke, secondhand smoke, vaping aerosol, chemicals, or fumes can irritate the nose, leading to inflammation and increased mucus production.
- Seasonal allergies: Seasonal allergies, also known as “hay fever,” can cause nasal inflammation and extra mucus. This creates an ideal environment for germs to grow.
- Other allergens: Other allergens that can cause sinusitis include dust mites, molds, cockroaches, and animal dander. Animal dander consists of tiny skin flakes from animals such as dogs and cats, which can float in the air and be inhaled. These skin cells contain secretions that can trigger allergic reactions, but animal fur or hair is not an allergen.
- Foreign objects in the nose: An object may become lodged in the nasal cavity and infected.
- Facial trauma: Injury may result in inflammation or infection.
Structural Factors
Structural issues in the nose or sinuses can disrupt the normal flow of mucus, leading to a buildup. Examples include:
- Nasal polyps: These noncancerous growths may block sinus openings if large enough.
- Deviated septum: The nasal septum is the cartilage wall separating the two sides of your nose. A deviated septum occurs when this wall is off-center or crooked.
- Cleft palate: A cleft palate is a birth condition where a baby has an opening in the roof of his or her mouth that creates a gap between the nose and mouth.
- Concha bullosa: Concha bullosa is an air-filled space within the concha or turbinate inside the nasal passage, usually in the middle part of the nose. It’s a common variation in the structure of the nose.
- Nasal bone spur: This may block a sinus opening.
- Tumors: A tumor in the nose or face may result in conditions that could cause a sinus infection.
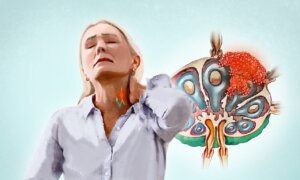
- Enlarged adenoids: Adenoids are lymph nodes in the throat that help trap germs entering the body through the nose. Enlarged adenoids can lead to problems such as acute rhinosinusitis, and in some cases, it can develop into chronic rhinosinusitis. Adenoids can become enlarged due to infection or may already be enlarged at birth.
- Ciliary dysfunction: The cilia in the sinuses are unable to move mucus effectively. This issue can impair mucous transport, leading to sinusitis.
- Sex: Women are more likely to develop sinus infections than men.
- Age: Children are the most prone to sinus infections. After children, sinus infections are more common in adolescents, then in people aged 25 to 64.
- Certain medications: Some medications, including birth control pills, drugs for high blood pressure or depression, and immunosuppressants, can worsen congestion and increase the risk of sinus issues.
- Underlying conditions: Certain medical conditions, such as asthma, AIDS, gastroesophageal reflux disease (GERD), cystic fibrosis, otitis media (middle-ear infection), and immune or autoimmune disorders, can increase the risk of sinus infection. People who develop dental infections or have allergic rhinitis are also more likely to experience sinus infections.
- Intensive care: People who spend prolonged periods lying on their backs in intensive care are more likely to have impaired mucociliary clearance.
- Pregnancy: Pregnant women are as many as six times more likely to experience acute sinusitis.
- Frequent colds: Young children with frequent colds are especially likely to be affected.
- Intranasal drug use: Chronic invasive fungal sinusitis is a rare but serious fungal infection that can affect people with normal immune systems. It can be associated with the inhalation of illicit drugs through the nose.
- Piloting aircraft and scuba diving: These individuals may experience barotrauma, injuries caused by air or water pressure changes. Barosinusitis is caused by sudden changes in air pressure that the body can’t adjust to. It can damage the sinus lining and usually causes facial pain or pressure.
- Prolonged oxygen use: Extended oxygen use, as with tubes inserted into the nose, can dry out the mucosal lining.
- Smoking: Cigarette smoke and nasal snuff significantly impair the nose’s ability to clear mucus. Research has also found that cotinine, a nicotine byproduct, slows the movement of cilia in nasal cells.
- Nasal decongestant sprays: Using these for more than two or three days in a row may increase the risk of developing a sinus infection.
- Severe burns: Inhalation injuries from burns significantly increase the risk of developing sinusitis.
- Computed tomography (CT) scan: A CT scan can help diagnose sinusitis and provide a closer look at the bones and tissues of the sinuses. It is typically used to assess the severity of sinusitis or to check for complications, such as a swollen, red eye.
- MRI: An MRI of the sinuses may be performed if a tumor or fungal infection is suspected.
- X-rays: If the patient has maxillary sinusitis, dental X-rays may be taken to check for a tooth abscess.
- Rhinoscopy (nasal endoscopy): Doctors or ear, nose, and throat (ENT) specialists may use a procedure called nasal endoscopy or rhinoscopy to examine the sinus openings and detect problems such as structural abnormalities. An endoscope is a thin, lighted tube inserted into the nose, often with a local anesthetic, to inspect the area and sometimes collect fluid samples for testing.
- Mucus culture: If a sinus infection is chronic or doesn’t improve after multiple rounds of antibiotics, a mucus culture may be performed to identify the cause of the infection. Most mucus samples are taken from the nose, but sometimes samples may be collected directly from the sinuses.
- Allergy testing: The doctor might refer the patient to an allergy specialist for skin prick testing to identify potential allergens.
- Blood tests: Blood tests for HIV or other tests for poor immune function may be requested by the doctor.
- Biopsy: Biopsies check for serious fungal sinus infections that may spread to nearby bone. A bone biopsy is needed to confirm this. Sinus tissue biopsies are taken using nasal endoscopes. These biopsies can also help diagnose rare conditions such as immotile cilia syndrome, which can lead to recurrent infections such as chronic sinusitis, bronchitis, and pneumonia.
- Ciliary function test: This test is used to diagnose primary ciliary dyskinesia, a genetic disorder affecting the cilia’s structure and function.
- Nasal cytology: Nasal cytology is a simple procedure used to examine the nasal lining by identifying and counting different cell types and their characteristics. It is performed by scraping the inside of the nose to collect a sample for analysis.
- Sweat tests: The sweat test measures the chloride levels in sweat and is the most reliable test for cystic fibrosis, which may be an underlying factor.
- Laryngitis: This is when the voice box gets inflamed.
- Dacryocystitis: This is when the eye’s tear sac gets inflamed or infected.
- Orbital cellulitis: This is a skin infection around the eye.
- Orbital abscess.
- Cavernous sinus thrombosis: This is a blood clot in the cave-like venous structure at the base of the brain.
- Meningitis.
- Epidural or subdural abscess or empyema: This is a collection of pus above or below the tough membrane covering the brain and spinal cord.
- Brain abscess (very rare).
- Bone infection.
- Spread of a bacterial infection.
- Facial cellulitis: This is inflammation or infection of the skin or underlying tissues of the face.
- Impaired vision.
- Blindness.
- Pain when moving the eye (limited eye movement).
- Seizures.
- Intense headache.
- Light sensitivity.
- Stiff neck.
- High fever.
- Trouble breathing, swallowing, or speaking.
- Confusion.
- Middle-ear infection: This is a more common complication, occurring much more often than 1 percent, especially in children.
- Temporary deafness.
- Death: While rare, this can occur due to a severe infection that develops in the orbit area, which holds the eyeball, or if the infection spreads to the brain.
- Apply a warm, damp washcloth to your face.
- Drink plenty of fluids.
- Use a humidifier.
- Avoid flying when feeling congested.
- Avoid extreme temperatures and sudden changes, as well as bending forward with your head down.
- Get plenty of rest, preferably lying on your side or propped up with a pillow to ease breathing.
- Avoid alcohol, as it can worsen sinus swelling.
- Avoid smoking.
Most people (about 70 percent) recover from an acute sinus infection without the need for prescribed medications. Watchful waiting allows two to three days to see if the immune system can resolve the condition without medications.
Medication
The goal of therapy for acute sinusitis is to improve drainage and control the infection. Medications can be used for this purpose. While chronic sinusitis is usually not curable, its symptoms can be effectively managed.
- Antibiotics: After a watchful waiting period of around 10 days, antibiotics may be prescribed if symptoms don’t improve. If a bacterial infection is the cause, antibiotics can help shorten the duration of acute sinusitis and lessen the severity of symptoms. Examples include trimethoprim-sulfamethoxazole, amoxicillin, and doxycycline. In some cases, antibiotics may be prescribed for up to three weeks. It’s important to complete the full course of medication as directed by the doctor.
- Nasal decongestant sprays: Nasal decongestant sprays (also known as topical vasoconstrictors) such as oxymetazoline and phenylephrine may temporarily relieve congestion but should not be used for more than two or three days to avoid rebound congestion (i.e., the nose remains constantly blocked unless the medication is used repeatedly), potential addiction, and long-term issues like persistent nasal dryness and crusting. Systemic vasoconstrictors, such as pseudoephedrine, are less effective and should not be given to young children and patients with hypertension, cardiovascular disease, hyperthyroidism, anxiety, and certain other medical conditions.
- Over-the-counter (OTC) pain relievers: Examples include aspirin, acetaminophen, and ibuprofen. Minors should not use aspirin.
- OTC cold medicine: Consult a doctor before using any OTC cold medicine, as some may worsen symptoms or cause side effects.
- Nasal steroids: Steroids delivered through a nasal spray can help reduce swelling inside the nose, typically showing effects within two or three days. Chronic sinusitis with polyps should be treated with topical nasal steroids. If symptoms are severe or don’t improve after 12 weeks, a short course of oral steroids may be considered.
- Mucolytics: Mucolytics, such as guaifenesin, may help thin mucus, making it easier to clear from the airways.
- Antihistamines: Antihistamines should be used only when allergies are involved.
- Leukotriene antagonists: Leukotriene antagonists, such as montelukast, zafirlukast, and zileuton, reduce inflammation through a mechanism different from glucocorticoids and are not used for all types of chronic rhinosinusitis. They are often effective for managing chronic sinusitis with nasal polyposis in people with coexisting asthma.
- Biologics: Biologics, such as dupilumab, omalizumab, and mepolizumab, target specific inflammatory pathways to reduce nasal polyps and improve chronic sinusitis symptoms. When used alongside steroid nasal sprays or washes, these medications are especially beneficial for patients with asthma or recurrent polyps after sinus surgery.
- Antifungal medications: These would be used in the case of a fungal infection rather than a bacterial infection.
Other Treatments
Nasal irrigation with saline (sterile saltwater solution) several times a day can reduce pain due to congestion and shorten symptoms. Devices such as syringes, neti pots, or sprayers can be used. Only use distilled, sterile, or boiled (and cooled) water for nasal irrigation to avoid harmful organisms in untreated tap water that can cause infections.
Surgery
When antibiotics fail, surgery may be needed to wash out the sinus, collect material for culture, or enhance sinus drainage, thus helping resolve inflammation. Surgery may also address nasal obstructions that hinder drainage.
1. Herbal Medicines
Phytotherapy involves using natural extracts as medicines or health agents, and it differs from standard pharmacology in that it preserves the plant’s complex substances with minimal processing. Phytotherapy has proven effective in alleviating symptoms of acute and chronic sinusitis in both children and adults, with high safety and tolerability.
- Sinupim: The herbal medicine Sinupim is an emulsion made from Pimpinella anisum seeds and sweet almond oil. In a 2016 study, 26 patients with chronic sinusitis without polyps received two drops of Sinupim in each nostril every 12 hours for four weeks. Their treatment results were significantly better than those of another group that received fluticasone nasal spray.
- English violet decoction: A 2019 study involving 30 patients with chronic sinusitis found that one type of English violet (Viola odorata) decoction could improve sinusitis symptoms more significantly than fluticasone propionate nasal spray.
- Angocin Anti-Infekt N: German herbal preparation Angocin Anti-Infekt N contains nasturtium and horseradish root. A 2007 study involving nearly 300 children aged 4 to 18 with acute sinusitis found that this herbal medicine was as effective as standard antibiotics but with fewer adverse events.
2. Nutrients
Two of the nutrients studied regarding their effect on sinusitis treatment are cineole and vitamin D.
3. Manuka Honey
Manuka honey can be effective against biofilm-producing bacteria. In a 2016 study, people with chronic rhinosinusitis (CRS) who had previously undergone sinus surgery used either Manuka honey or saline for sinus irrigations twice a day for 30 days, along with other treatments such as antibiotics or steroids if needed. The results showed that the honey group had more negative cultures (bacteria-free) posttreatment, especially for those not using antibiotics or steroids. However, the difference did not reach clinical significance. The researchers suggested Manuka honey might be an effective treatment for CRS flare-ups on its own.
4. Acupuncture
As per a 2022 meta-analysis, acupuncture, whether used alone or as a complementary treatment for chronic sinusitis, was linked to symptom improvements with no risk of serious adverse events. However, the researchers noted that the high degree of similarity among the clinical trials reviewed and their moderate-to-low quality warrant more research to confirm the findings.
5. Yoga
Yogic practices are believed to bolster resistance to sinus infections and prevent and treat sinusitis. Some researchers believe correctly practicing yogic techniques can potentially clear sinus impurities and prevent further blockages. In a 2018 study, 20 sinusitis patients received yoga therapy over six months. The therapy reduced the sinus inflammation in all participating patients and improved their resistance to infection.
- Wash your hands frequently.
- Avoid close contact with people who have colds or infections.
- Avoid cigarette smoke and secondhand smoke.
- Receive allergy shots if needed. Additionally, allergy testing can identify environmental triggers that chronic sinusitis patients should avoid.
- Use a clean humidifier with filtered water to moisten the air at home, especially in cold, dry climates.
- When possible, avoid allergens or irritants that trigger nasal allergies.
- Limit touching your face with unclean hands and limit exposure to infections during the cold season.
- Follow a healthy lifestyle to maintain a strong immune system and prevent repeated sinus infections. A healthy lifestyle includes sleeping seven or eight hours nightly, eating a balanced, whole-food diet, managing stress, and exercising regularly.
- Drink plenty of water to keep mucus thin.