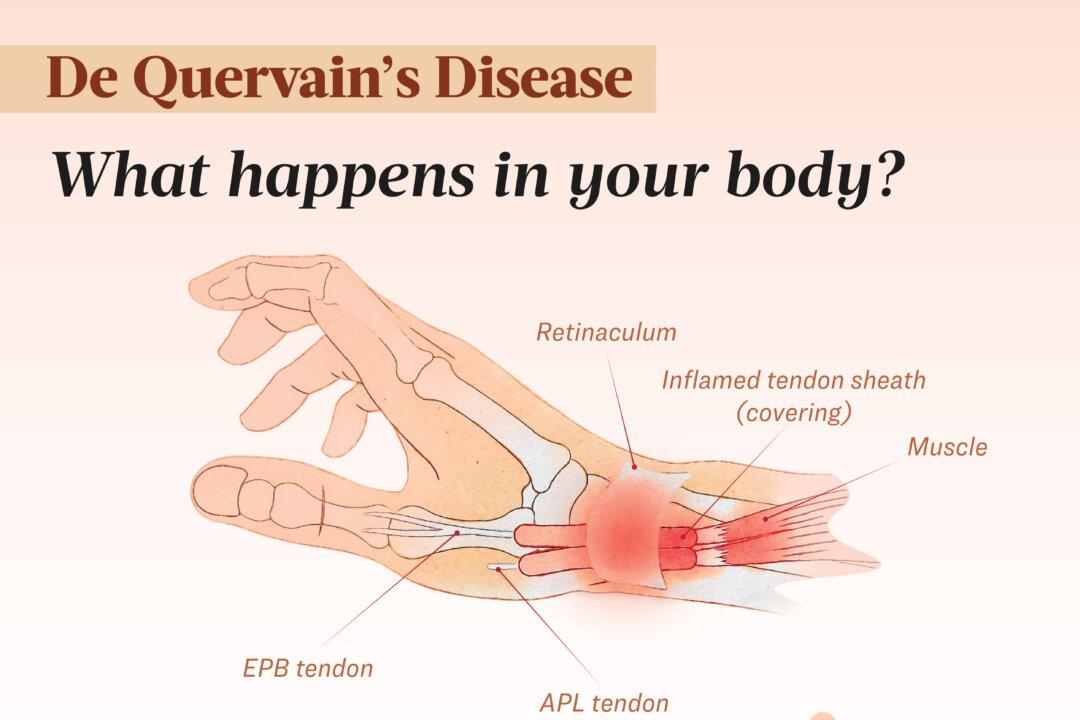
- Type I: Characterized by a thickening and tight constriction of the APL and EPB tendons by a loop-shaped retinaculum or connective tissue, with no separation between them.
- Type II: The retinaculum compresses only the EPB, leaving a clear separation.
Identifying the two distinct forms may influence treatment approaches.
Risk Factors
The development of dQD is thought to be linked to several factors. Potential causes include:
- Repetitive hand movements: Performing repeated wrist and thumb motions may lead to inflammation and progressive narrowing of the tendon tunnel
- Overuse of wrist and thumb: Prolonged overuse can result in chronic tendon injuries over time
- Acute wrist injury: A fall or impact may cause scar tissue to form, limiting tendon movement
- Inflammatory conditions: Conditions such as rheumatoid arthritis or diabetes, which cause swelling and pain, can contribute to tendon inflammation
- Anatomical differences in the wrist: Features like extra compartments in the tendon sheath or multiple tendon branches in the thumb muscles may increase the risk of dQD
Additional Risk Factors
Beyond repetitive movements and injuries, several other factors may increase the likelihood of developing dQD. These include biological differences, life events, and certain medical conditions that contribute to tendon irritation and wrist strain.
- Sex: dQD is several times more common in women than in men
- Age: dQD is more common between ages 40 and 59, though it can occur at any age
- Childbirth: The largest group of dQD patients are women with young babies, especially those who are breastfeeding. It typically develops four to six weeks after childbirth. While the cause is unclear, it may be related to hormonal changes or the physical strain of lifting and feeding the baby. Symptoms usually resolve once a mother lifts her child less frequently
- Aromatase inhibitor therapy: Patients receiving this treatment for breast cancer may be at increased risk
- Pregnancy: Hormonal fluctuations during pregnancy and postpartum can cause fluid retention and swelling in the tissues, including the tendon sheaths in the wrist
- Certain sports: Activities such as tennis, racquetball, squash, and skiing involve repetitive, forceful movements that stress the thumb and wrist
- Pain: The primary symptom is pain on the thumb side of the wrist, which may develop gradually or suddenly. The pain often starts in the wrist and can extend up the forearm, worsening with activities such as grasping, lifting, using scissors, turning a door handle, gaming, or twisting the wrist. The pain may be sharp or dull.
- Swelling: The thumb side of the wrist may become puffy or inflamed and can sometimes develop a fluid-filled cyst—a small sac of tissue in the area.
- Catching sensation: A catching or snapping feeling may occur when moving the thumb. Some people hear a strange sound, such as a squeak, crackle, snap, or creak, when moving the wrist or thumb.
- Stiffness: Pain and swelling can make it challenging to move the thumb and wrist.
- Tenderness: The area just above the bony bump on the wrist may be sore to the touch due to irritated tendons.
- Numbness: The back of the thumb and index finger may feel numb.
- Small bump: A small bump may develop on the thumb side of the wrist.
1. Medical History
The diagnostic process starts with a medical history and physical exam. The doctor checks for past symptoms, overuse injuries, repetitive hand movements, hand dominance, and pregnancy or postpartum status.
2. Physical Exam
The doctor examines the hand for swelling, tenderness, or numbness around the base of the thumb and checks for crackling or popping sounds when the thumb moves. Pressure may be applied to the wrist near the base of the thumb to assess pain and swelling.
3. Imaging Tests
To help diagnose dQD, clinicians may use imaging tools such as ultrasound and X-ray. Ultrasound can visualize inflamed tendons and help confirm the condition, while X-rays are useful for ruling out other causes of radial wrist pain, such as osteoarthritis of the thumb carpometacarpal joint.
Tier I: Conservative Management
- Patient education: Avoid repetitive or strain-inducing movements
- Rest: Limit wrist and thumb movements, avoiding activities that worsen symptoms
- Cold/heat therapy: Apply ice for 20 minutes every four hours or heat for 15 minutes every four to six hours
- Kinesiotaping: Can help reduce pain and swelling, support movement, and provide stability
- Nonsteroidal anti-inflammatory drugs: Reduce swelling and relieve pain
- Thumb splinting: May provide temporary relief, but recurrence rates are high, and patient compliance is often low
- Immobilization: Wearing a rigid splint to keep the wrist still can help relieve pain for people with mild symptoms
- Physical therapy or exercises: Stretch, strengthen, and increase the range of motion in the wrist and thumb. Following the splinting period, if symptoms have significantly improved, a hand therapist may recommend an exercise program, including assisted thumb extension, abduction, and wrist deviation; active thumb extension and abduction; and isometric wrist holds, thumb strengthening, and resisted wrist deviation
- Occupational therapy: Learning to perform tasks with a splint
- Therapeutic ultrasound: Used to treat inflamed tendons
- Extracorporeal shockwave therapy: A noninvasive procedure that uses sound waves to promote healing
- Transcutaneous electrical nerve stimulation: Uses mild electrical currents for pain relief
Tier II: Corticosteroid Injections
One injection works for about half of patients, with a second helping another 40 to 45 percent. Ultrasound guidance can improve effectiveness. Potential complications include skin thinning, discoloration, and, rarely, tendon weakening.
Tier III: Surgery
Most patients find success with nonsurgical treatments. Surgery is considered a last resort for persistent symptoms. In these cases, De Quervain’s tendon release surgery may be recommended.
- Worsened symptoms: Without treatment, pain and other symptoms may persist or worsen. Over time, dQD can become chronic, making it difficult to use the wrist and thumb for everyday activities.
- Permanently limited movements: The progressive and chronic nature of the inflammation can lead to lasting restrictions in wrist and thumb mobility.
- Tendon sheath bursting: Untreated inflammation leads to a continuous narrowing of the tendon sheath, increasing friction between the tendons and the sheath during movement. This constant friction can cause the tendons to degenerate and weaken, leading to tears in the tendon fibers.
While most patients recover well, dQD surgery carries some risks, including:
- Nerve injury or damage, causing numbness and tenderness
- Tendon entrapment or dislocation
- Wound complications, like swelling, bruising, bleeding, or infection
- Scarring
- Stiffness
- Complex regional pain syndrome
- Abnormal tendon movement
Ayurvedic Management
One of the world’s oldest medical systems, Ayurveda combines plant-based products (along with some animal, metal, and mineral sources), diet, exercise, and lifestyle practices for treatment.
Massage Therapy
Massage treatment, particularly deep transverse friction applied to the APL and EPB tendons, may relieve dQD symptoms. While there is debate about whether massage can break up tendon adhesions, friction techniques may reduce fibrous adhesion and increase the activity of fibroblasts—cells important to wound healing and tissue repair—leading to less pain and improved function.
Acupuncture
A 2014 study involving 30 dQD patients compared acupuncture with corticosteroid injections. One group of participants received five 30-minute acupuncture sessions targeting several acupuncture points, while the other received a methylprednisolone acetate injection in the first dorsal compartment of the wrist. Both groups showed short-term improvement in pain and function, though the corticosteroid injection demonstrated a slightly higher success rate.
Moxibustion
This treatment involves burning materials called moxa to stimulate the patient’s immune system. The moxa is placed on the skin over acupuncture points or at the end of an acupuncture needle. The heat generated is believed to penetrate deep into the body and activate the immune system.
- Avoid repetitive movements: Minimize repetitive wrist movements and modify actions to reduce stress. Also, ensure correct technique when performing repetitive hand and wrist movements to avoid strain.
- Take breaks: Avoid overuse by taking frequent breaks during activities involving repetitive thumb movements.
- Strengthen forearms: Strengthening forearm muscles improves wrist stability and reduces stress on tendons.
- Wear a brace or splint: If necessary, use a splint or brace to support the thumb and wrist.
- Follow recommended exercises: Perform exercises suggested by a physical therapist to stretch the thumb and wrist and relieve pressure.








