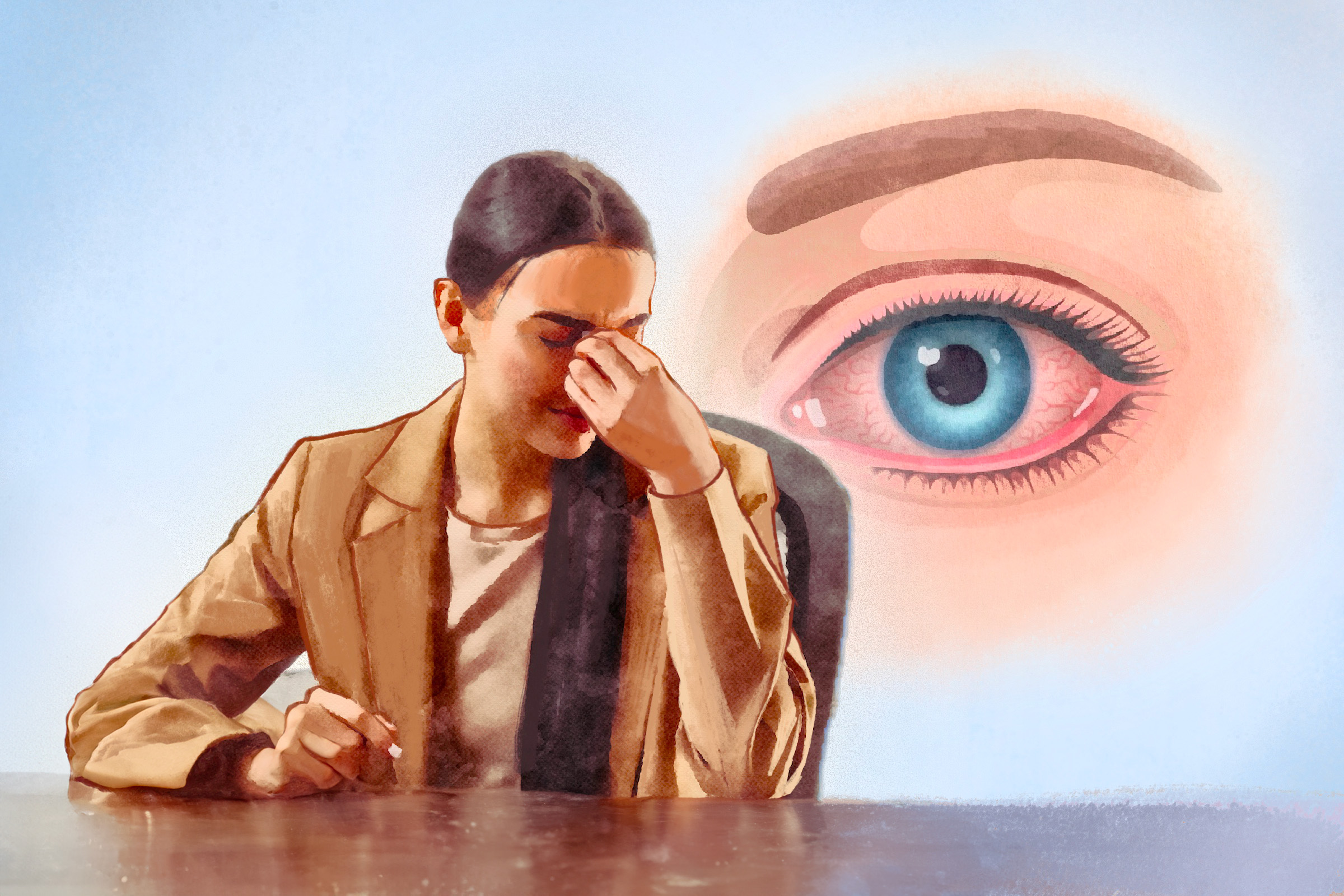
Common Sensations and Discomfort
Many people with dry eyes describe a gritty, burning, or stinging sensation in their eyes as if something is stuck inside. Some also experience pressure behind the eyes or sharp, stabbing pain. A heavy feeling in the eyelids or difficulty keeping the eyes open can also occur, especially after prolonged use of screens.
Vision-Related Symptoms
Blurred vision—particularly when it fluctuates—can be an early sign of dry eye. Sensitivity to light is also common and may make it uncomfortable to be in bright environments. Frequent blinking or excessive tearing can paradoxically signal dryness, as the eyes may produce extra tears in response to irritation.
Changes in Eyelids and Tear Production
Dry eye can also affect the eyelids, leading to eyelid twitching, inflammation, or a lack of tears when crying. Some people may notice crusting or clumping of the eyelashes, particularly upon waking.
Additional Symptoms
Redness is a common sign of dry eye and may worsen with certain over-the-counter eye drops, which temporarily shrink blood vessels to reduce redness. However, once the effect wears off, the redness can return even stronger. Many people also experience discomfort while using digital devices, as prolonged screen time reduces blinking, which can increase dryness and irritation.
- Oily layer (lipid layer): This outer layer of tears is produced by the meibomian glands (oil glands along the edge of the eyelids). It smooths the tear surface and prevents the two inner layers from evaporating too quickly, helping maintain clear vision.
- Watery layer (aqueous layer): This middle layer is produced by the lacrimal glands (tear glands located above the outer corners of the eyes). It hydrates the eye, removes bacteria and debris, and makes up the majority of visible tears.
- Mucus layer (basal layer): This innermost layer is produced by the conjunctiva (a thin, transparent membrane covering the white part of the eye and the inner eyelids). It helps tears adhere to the eye’s surface, spreads the watery layer, and provides lubrication to keep the eye moist.
When any of these layers are disrupted, the quality of the tear film is compromised, making the eye more susceptible to dry eye disease.
- Aqueous tear-deficient dry eye: This type occurs when your eyes don’t produce enough tears. It can result from various factors, including aging, hormonal changes, autoimmune diseases, and certain medications. It most commonly occurs in postmenopausal women for unknown reasons and is frequently associated with Sjögren’s syndrome, rheumatoid arthritis, or systemic lupus erythematosus.
- Evaporative dry eye: This type occurs when tears evaporate too quickly due to a lack of a proper oil layer on the surface of the watery part of the tears. It is often caused by meibomian gland dysfunction, a condition in which the glands in your eyelids that produce oil don’t work properly. The oil in tears helps prevent them from evaporating too quickly.
It is possible to have both aqueous tear-deficient dry eye and evaporative dry eye at the same time. This is called mixed dry eye.
- Age: Tear production decreases as people get older.
- Gender: Dry eye syndrome is more common in women, especially those over 50.
- Dry or polluted environments: Environmental factors such as dry air in heated rooms during winter, air-conditioned rooms in summer, smoky surroundings, and irritants like chemical fumes, cigarette smoke, and pollution can trigger dry eye symptoms. Strong winds (e.g., sleeping with a fan or using a sleep apnea mask), high temperatures, high altitudes, and low humidity can also contribute to dry eye.
- Certain conditions: Many underlying conditions can lead to dry eye. Notable autoimmune conditions include Sjögren’s syndrome, Graves’ ophthalmopathy, and connective tissue disorders. Other conditions that increase risk include diabetes, multiple sclerosis, blepharitis (eyelid inflammation), and facial paralysis, such as Bell’s palsy.
- Medications: Certain medications can contribute to dry eye, including antihistamines (anti-allergy medication), contraceptive pills, high blood pressure medicines, benzodiazepines, diuretics, hormone replacement therapy, inhaled corticosteroids, isotretinoin (used to treat severe acne), glaucoma drops, and antidepressants.
- Conjunctival scarring: Chemical burns and conditions like Stevens-Johnson syndrome (caused by a reaction to certain medications) can lead to conjunctival scarring, increasing the risk of dry eye.
- Certain herbal products: Herbal supplements like kava and echinacea have been linked to dry eye.
- Laser eye surgery (LASIK): Some individuals experience dry eyes after LASIK due to damage to the corneal nerves. While these nerves typically regenerate and symptoms improve over time, dryness may persist in some cases. People with preexisting dry eye syndrome should avoid LASIK, which can worsen the condition.
- Computer vision syndrome: Prolonged screen time reduces blink frequency, leading to dry eyes.
- Contact lenses: Contact lenses absorb tears, increasing the risk of dryness.
- Nutrient deficiencies: Deficiencies in vitamin A and omega-3 fatty acids can contribute to dry eye. These deficiencies may be caused by underlying medical conditions, such as digestive disorders.
- Alcohol: A 2021 study found that alcohol use is a risk factor for dry eye disease, but the effect was observed only in females.
- Poor sleep quality: A 2019 study found a strong link between poor sleep quality and more severe dry eye symptoms.
Comprehensive Eye Exam
The examination should assess the face, eyelids, blinking patterns, eyelid margins, eyelashes, conjunctiva, cornea, and tear film.
Diagnostic Tests
Ophthalmologists use several tests to diagnose dry eye syndrome and check for corneal damage, including:
- Examining overall eye health: A slit lamp test provides an overall assessment of eye health and allows ophthalmologists to assess the eye’s structures under magnification, helping detect abnormalities in the cornea, conjunctiva, eyelids, and tear film.
- Measuring tear production: The Schirmer test involves placing a small strip of filter paper inside the lower eyelid to measure tear volume over a few minutes, while the phenol red thread test uses a pH-sensitive thread to assess tear production.
- Assessing tear quality and evaporation: Tear break-up time involves applying a dye to the eyes to measure how long tears remain stable before evaporating, while tear film osmolarity analyzes a small sample of tears to determine the salt concentration, which can indicate tear film instability.
- Staining the eye’s surface to detect damaged cells: Epithelial staining uses special dyes to highlight areas of cell damage on the eye’s surface using specific stains like fluorescein sodium, rose bengal, and lissamine green.
- Corneal abrasions: The cornea is prone to scratches from dust, hair, or other foreign objects, especially when lubrication is minimal. Painful abrasions can also occur if the eyelid sticks to the cornea, such as upon waking.
- Corneal scarring: Although minor corneal abrasions usually heal in a few days, deep or poorly healed abrasions may cause permanent corneal scarring, leading to blurry or reduced vision as scarring prevents light from properly entering the eye.
- Corneal ulceration: A corneal ulcer is an open sore on the cornea. It can be treated with antibiotic eye drops, but if left untreated, it can spread, damage the eye, and lead to partial or total blindness.
- Infections: Corneal abrasions may result in infections, such as infectious keratitis, which can cause pain, redness, and vision problems.
- Vision fluctuations: Blurred or unstable vision may occur due to inconsistent tear film quality, making it harder to focus.
- Vision loss: Severe or untreated dry eye may lead to long-term damage and permanent vision impairment.
- Debilitating eye discomfort: Persistent dryness, irritation, and pain can interfere with daily activities and reduce quality of life.
- Conjunctivitis: This is inflammation of the conjunctiva, the transparent membrane covering the white part of the eyeball and inner eyelids. Most cases are mild and resolve without requiring specific treatment.
- Vascularization: This is the abnormal growth of blood vessels in the cornea, which can interfere with vision.
- Inability to wear contact lenses: Dry eyes can cause discomfort and irritation, making it difficult or impossible to tolerate contact lenses.
- Depression: Research has found that women with dry eyes are more prone to negative moods, anxiety, and psychological stress.
1. Home-Care and First-Line Treatments
These treatments are typically recommended for mild symptoms and focus on lifestyle changes to reduce eye dryness:
- Taking regular breaks from screen use, reading, or TV to encourage blinking
- Allowing eyes to rest and stay lubricated to prevent tear film evaporation
- Reducing exposure to direct airflow, fans, or wind
- Using a humidifier to maintain moisture in the air
- Drinking eight to 10 glasses of water daily to stay hydrated
- Getting seven to eight hours of sleep each night to support eye health
There are also certain self-care measures that you can take to alleviate dry eye symptoms. In the case of dry eyes caused by computer vision syndrome, consider doing the following:
- Position the screen 15 to 20 degrees below eye level to reduce dryness from more open eyelids and minimize neck strain.
- Adjust screen brightness to match surrounding light for greater comfort.
- Increase font size to reduce eye strain and minimize the need for intense focus.
- Use sans serif fonts, which are easier on the eyes.
- Take breaks every hour or two by blinking or briefly closing your eyes.
Other self-care measures include:
- Avoid certain eye drops: Steer clear of eye drops containing redness relievers or allergy ingredients, such as Visine, Similasan, or Naphcon A.
- Use gel drops or ointments: If sleeping with a fan or in moving air, use gel drops or eye ointment before bed to keep the eyes moist overnight.
- Avoid smoking and secondhand smoke: Smoke exposure can worsen dryness and irritation.
- Refrain from using eye makeup: Avoid wearing eye makeup when experiencing infection, inflammation, or sore eyes.
- Massage the eyelids: Apply a warm, moist cloth to your eyelids for five minutes each morning, then gently massage the eyelids to help boost the eyes’ natural moisture.
- Use eyelid cleaners: This includes warm compresses and lid scrubs. Applying a warm compress at night can help stimulate tear production and clear clogged meibomian glands, especially for those with blepharitis. An eyelid scrub involves gently applying a cleansing solution to the eyelid to remove excess oil and debris. Eyelids can be gently cleaned with diluted baby shampoo or eyelid margin scrubs while keeping the eyes closed.
2. Second-Line and Advanced Treatments
If first-line treatments are insufficient, the following options may be considered.
Punctal Plugs
These are small devices inserted into the tear drainage ducts to slow tear drainage, keeping the eyes moist for longer. This minimally invasive, painless procedure requires no recovery time. Side effects, such as excessive tearing or mild irritation, are rare, and most people do not notice the plugs at all.
Night-Time Ointment or Moisture Goggles
Lubricating ointments, applied before bed, provide longer-lasting moisture and help prevent morning dryness, though they are typically not used during the day as they can blur vision. Moisture chamber goggles help reduce tear evaporation by increasing local humidity and minimizing airflow, effectively stabilizing the tear film and slowing down tear loss.
Thermal Pulsation Therapy
This treatment uses specialized devices that deliver controlled heat and massage to the eyelids, helping break down blockages in the meibomian glands and improving oil secretion.
Intense Pulsed Light Therapy
Nonlaser light energy is used on the eyelid skin to clear blockages in the meibomian glands, enhance oil flow, reduce eyelid redness, and minimize spider veins.
3. Medications
Doctors may prescribe various medicated eye drops to manage inflammation and symptoms of blepharitis or dry eye, including:
- Cyclosporine eye drops: These are anti-inflammatory drops for long-term treatment of dry eye, targeting inflammation of the lacrimal gland. Relief may take three months or longer, although some patients improve sooner.
- Corticosteroid eye drops: These drops are a short-term treatment option for inflammation-related dry eye.
- Lifitegrast eye drops: These drops reduce inflammation associated with dry eye disease.
- Antibiotics: Oral antibiotics (e.g., doxycycline, macrolide, and tetracycline) and topical antibiotics (e.g., erythromycin ointment and azithromycin eye drops) are used to treat dry eye. Doxycycline is not recommended for pregnant or nursing mothers.
Over-the-counter solutions include oral essential fatty acid supplements, which may help manage dry eye symptoms due to their anti-inflammatory properties. Artificial tears are topical ocular lubricants that supplement the natural tear film to keep eyes moist. These over-the-counter eye drops are typically used two to four times daily and come in various strengths, including preservative-free options for sensitive individuals. Special formulations are also available for contact lens wearers.
4. Surgical Interventions
For cases of severe or persistent dry eye that do not respond to other treatments, surgical options may be considered to help retain moisture and improve eye comfort. These procedures aim to reduce tear drainage, enhance eyelid function, or protect the eye’s surface.
- Surgical punctal occlusion: In this procedure, an ophthalmologist applies heat to the puncta (small tear openings in the inner corners of the eyelids) in each eye, permanently closing the tear ducts to prevent tears from draining.
- Tarsorrhaphy: If the eyelids do not close properly, a procedure called lateral tarsorrhaphy can be performed. This surgery involves stitching the outer edges of the eyelids together to improve eye closure and moisture retention.
- Eyelid Surgery: In some cases, dry eye may occur if the lower eyelids are too loose, causing tears to drain too quickly. A surgical procedure may help correct the eyelids and retain tears on the eye’s surface. However, this treatment is rare.
5. Other Treatments
These treatments are typically reserved for severe dry eye cases that don’t respond to other therapies.
- Serum eye drops: In severe cases, autologous serum drops may be recommended. This involves drawing the patient’s blood, processing it to remove blood cells, and using the resulting serum as eye drops for the eye surface. Serum eye drops contain growth factors and essential nutrients that help reduce dry eye symptoms.
- Therapeutic contact lenses: Scleral lenses are specialized contact lenses designed to keep the eye’s surface moisturized. These lenses are larger than regular contact lenses, covering the cornea and resting on the sclera (the white part of the eye) to provide continuous hydration.
- Amniotic membrane grafting: The amniotic membrane serves as a basement membrane substitute or temporary graft in the eye. It has anti-inflammatory and anti-scarring properties and contains growth factors that aid in epithelial wound healing. Cryopreserved amniotic membranes have been shown to restore corneal epithelial health, improve visual acuity in dry eye conditions, and alleviate symptoms of dry eye syndrome.
- Yoga
- Qigong
- Aerobic exercise
- Social connections
- Maintaining a positive outlook
1. Herbal Formulations
- Chi Ju Di Huang Wan: A traditional Chinese herbal formula made with goji berry, chrysanthemum, and Rehmannia. A 2005 study found that it improved tear film and corneal health in dry eye patients.
- Si Wu Tang: Also known as Four-Substance Decoction, this classic formula contains four herbs: Rehmannia, female ginseng (Angelica sinensis), Chinese peony, and Ligusticum. A small 2020 study found that combining two traditional Chinese herbal formulas (Chi Ju Di Huang Wan and Si Wu Tang) significantly improved tear production and relieved dry eye symptoms in patients after three months.
- Sea buckthorn oil: Rich in anti-inflammatory and antioxidant compounds, sea buckthorn oil improved dry eye symptoms and helped stabilize the tear film in a 2010 study.
2. Herbal Supplements
Maqui berry (Aristotelia chilensis): Maqui is an evergreen shrub native to Chile and other parts of South America. A 2023 study found that taking maqui berry extract reduced ocular surface inflammation and improved dry eye signs and symptoms in patients.
3. Acupuncture
A 2019 study involving 24 patients with dry eye syndrome found that one week of acupuncture treatment improved symptoms. Researchers concluded that acupuncture provides a true therapeutic effect, rather than just a placebo response, making it a potential complement to routine clinical treatment for dry eye.
4. Auricular Acupressure
A 2017 study involving 50 dry eye patients tested auricular acupressure with electrical stimulation at four points on both ears, which was performed twice a week for four weeks.
5. Moxibustion
Moxibustion is a traditional Chinese medicine therapy that involves burning dried mugwort (moxa) on specific points of the body.
- Wear wrap-around glasses to shield your eyes from wind, hot air, sunlight, and smoke.
- Avoid using a hairdryer when possible.
- Increase humidity indoors by placing a pan of water near a heater or radiator during winter.
- Avoid smoking and limit alcohol consumption.
- Reduce contact lens wear by limiting the number of hours you wear them daily.
- Include omega-3 fatty acids in your diet to support eye health.
- Prevent and manage blepharitis by cleaning your eyelids, removing makeup nightly, and managing underlying skin conditions.
- Address other medical conditions that contribute to dry eye.
- Protect your eyes when exposed to dust or chemical irritants.