Not all antidepressants are created equal when it comes to your waistline, heart, and blood pressure, according to a sweeping study published in The Lancet that analyzed data from more than 58,000 people to create the first comprehensive ranking of drug side effects.
The analysis compared 30 antidepressants, some of which are not available in the United States, from older tricyclics such as amitriptyline to newer selective serotonin reuptake inhibitors (SSRIs) such as sertraline (Zoloft).
Experts said that the side effects listed are not new or surprising.
The study affirmed well-known observations about antidepressant side effects, Dr. Joseph Goldberg, a clinical professor of psychiatry at the Icahn School of Medicine at Mount Sinai, who was not involved in the study, told The Epoch Times in an email.
What’s new, Goldberg noted, is the comprehensive review of the literature that reassures us, and helpfully quantifies for us, that many of these common side effects tend to have only modest impacts.
The findings reinforce the need for personalized choices and regular monitoring, especially for long-term users, because side effects can build over time.
Weight Gain, Blood Pressure, and Cholesterol Changes
People on antidepressants experienced a nine-pound difference in weight change across drugs.
The most extreme weight changes occurred in those taking agomelatine (Valdoxan) and maprotiline (Ludiomil), with the former associated with a weight loss of about five pounds and the latter with a weight gain of about four pounds.
Both of these drugs, however, are not approved for use in the United States.
Differences in heart rates exceeded 20 beats per minute, from fluvoxamine (Luvox), which slowed the heart by calming the nervous system, to nortriptyline (Pamelor), a stimulant that increased heart rates.
Blood pressure shifts were also notable, with the upper (systolic) number differing by about 11 points between certain tricyclics such as nortriptyline and doxepin (Silenor). These drugs directly act on the body’s nervous system and blood vessel receptors, which can raise or lower blood pressure.
“These are not alarming effects,” Dr. Daniel Carlat, a psychiatrist and chair of the psychiatry department at MelroseWakefield Healthcare, part of the Tufts Medicine network, who was not involved in the study, wrote in an email to The Epoch Times, “but the paper reinforces the value of simple monitoring—blood pressure, weight, and labs—especially for patients with heart or metabolic risk.”
“Some of the serotonin-norepinephrine reuptake inhibitors—like duloxetine and venlafaxine—caused small but measurable increases in blood pressure and cholesterol, which makes it worth checking those numbers periodically.”
For people with diabetes, hypertension, or heart problems, small increases in weight gain and heart measurements can affect blood sugar levels or add strain to the heart and blood-vessel system.
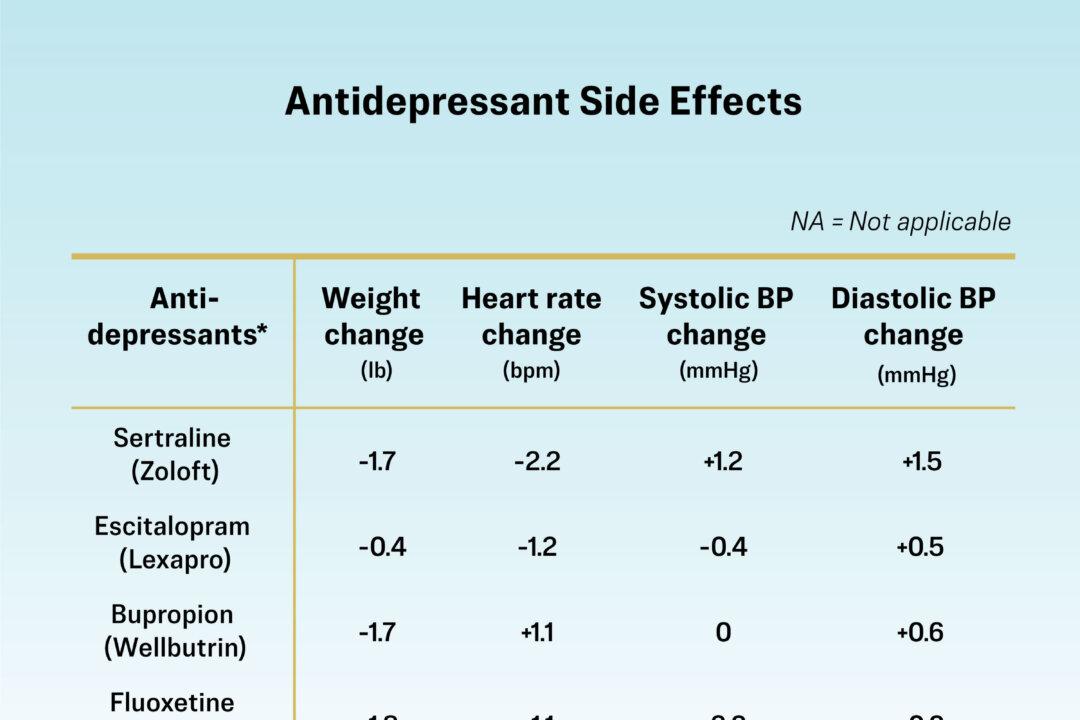
Common Antidepressants and Potential Side Effects
The following is not a complete list of potential side effects, and the effects listed vary by person, with not everyone experiencing them.
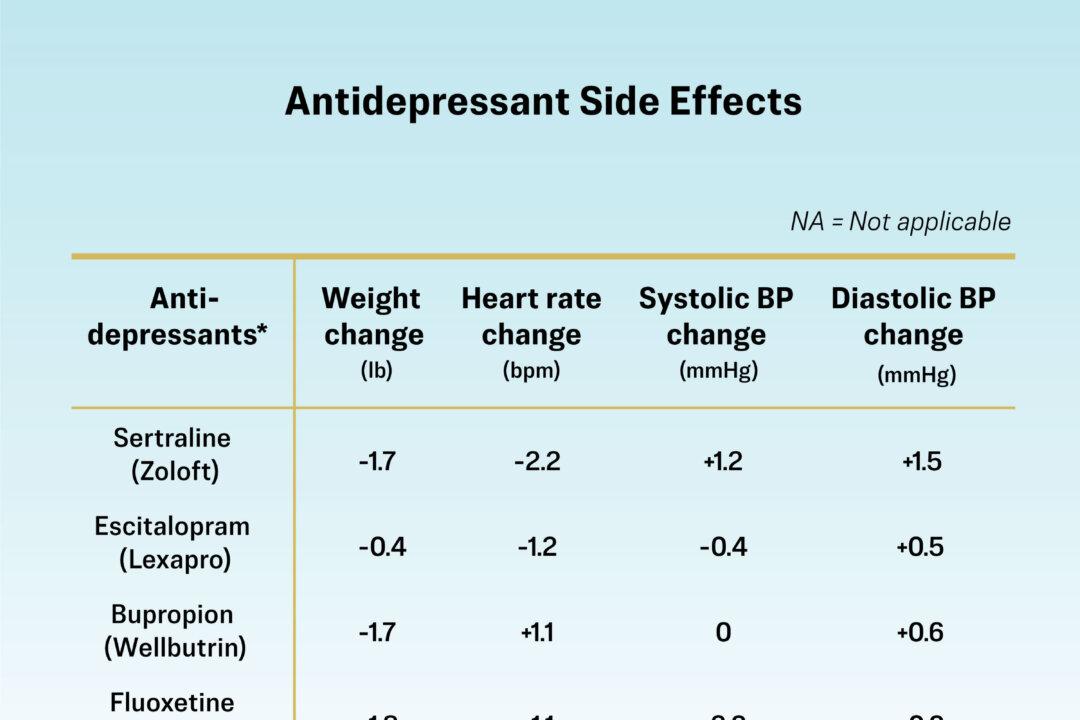
(The Epoch Times)
Why Different Drugs Have Different Effects
About 20 million Americans take antidepressants for depression or anxiety. Beyond mood, these drugs can influence your metabolism, often in very different ways.
Antidepressants affect brain chemicals that lift mood—the same chemicals that regulate appetite, metabolism, blood vessels, and the heartbeat.
Depending on the specific medication, appetite may increase or decrease, blood vessels may relax or constrict, and the heart’s rate may shift slightly.
For example, agomelatine, which causes weight loss and regulates the sleep-wake cycle, may help reduce appetite, while maprotiline, which is linked with weight gain, increases appetite.
Outside of drug side effects, weight gain can also occur when an antidepressant lifts mood—people who were eating less due to depression may return to their usual appetite.
Side effects aren’t the same for everyone, which is why it’s important to consider a person’s overall health, symptoms, and sensitivities when choosing a treatment.
Risks Versus Benefits
“Side effects are not necessarily equal-opportunity offenders,” Goldberg said. “Every patient is unique, and almost all medications carry some side effects—even placebos.”
Some antidepressants that are more effective at treating difficult-to-treat depression carry a higher risk of weight gain, and it would be a disservice to patients if their doctor were to avoid prescribing them simply because of a higher risk of weight gain, Goldberg said.
The patient would be at risk of persistent depression, having functional impairment, and possibly even suicide if their depression went untreated.
“It all starts with a conversation about whether the depression is severe enough to merit medication versus therapy,” Carlat said. “If we do decide to try a medication, I start with those that offer the best balance of benefit and tolerability—typically an SSRI like sertraline or escitalopram. Bupropion is also high on my list because it rarely causes sexual side-effects or weight gain.”
In children and young adults, antidepressants can provoke or exacerbate suicidal thoughts, while older adults appear to be somewhat protected from this side effect, Goldberg said. Additionally, patients with anxiety may also be more prone to developing such side effects.
Some symptoms of depression may also overlap with side effects from medication, Goldberg said. Appetite changes, weight gain, and sexual issues can stem from either depression or medication use.
Clinicians, therefore, need to consider all factors and make personal decisions for each patient. Maintaining open communication between patients and doctors is essential.
Age, anxiety level, genetics, and the use of multiple medications also influence side effect risk. The study did not address why some people are more vulnerable to side effects than others, or how clinicians can identify higher-risk patients.
What to Know Before Starting an Antidepressant
According to Goldberg and Carlat, for patients considering antidepressants, shared decision-making with doctors is key. Common concerns, according to the study’s researchers, include:
- High Blood Pressure: Ask about medications known to raise blood pressure, such as amitriptyline or venlafaxine.
- Weight Gain: Options such as agomelatine, sertraline, or venlafaxine may lead to smaller average weight changes.
- Cholesterol: Some SSRIs, such as citalopram and escitalopram, appeared more neutral on cholesterol compared with paroxetine or duloxetine.
- Usage Period: Ask questions such as “How long will I need this medication?” and “Are there non-drug options—such as group therapy or exercise—that could work as well?”
Because most of the trials covered in the study lasted only eight weeks, the long-term physical effects of antidepressants remain uncertain, thus experts recommend routine checks of weight, blood pressure, heart rate, and cholesterol for anyone on long-term therapy.
“There are seldom absolutes,” Goldberg said. “A person with high risk for heart disease may be a poorer candidate for a drug that causes weight gain or raises blood sugar.”