A baby’s gut bacteria in its first week of life could be the key to avoiding hospital stays later—at least when it comes to serious lung infections.
A new study of nearly 1,100 newborns found that infants with specific beneficial bacteria were significantly less likely to be hospitalized for viral respiratory illnesses during their first two years.
“Our research raises the possibility that certain early gut microbiomes might help lower this risk [of respiratory infections],” study lead author Dr. Cristina Garcia-Mauriño said in a statement. Given that viral lower respiratory tract infections are among the leading causes of hospitalization in young children, she said these findings could have significant implications for infant health.
The study, recently published in The Lancet Microbe, is the first to link the makeup of a baby’s gut bacteria—the collection of bacteria that begins forming immediately after birth, known as the microbiome—in the first week of life to hospital visits for respiratory infections in early childhood.
Key Findings
Researchers from University College London and the Wellcome Trust Sanger Institute collected stool samples from nearly 1,100 newborns within their first week of life. Using advanced genetic testing, they analyzed the bacterial composition and then tracked each child’s health records for two years, focusing on hospital admissions for viral lung illnesses.
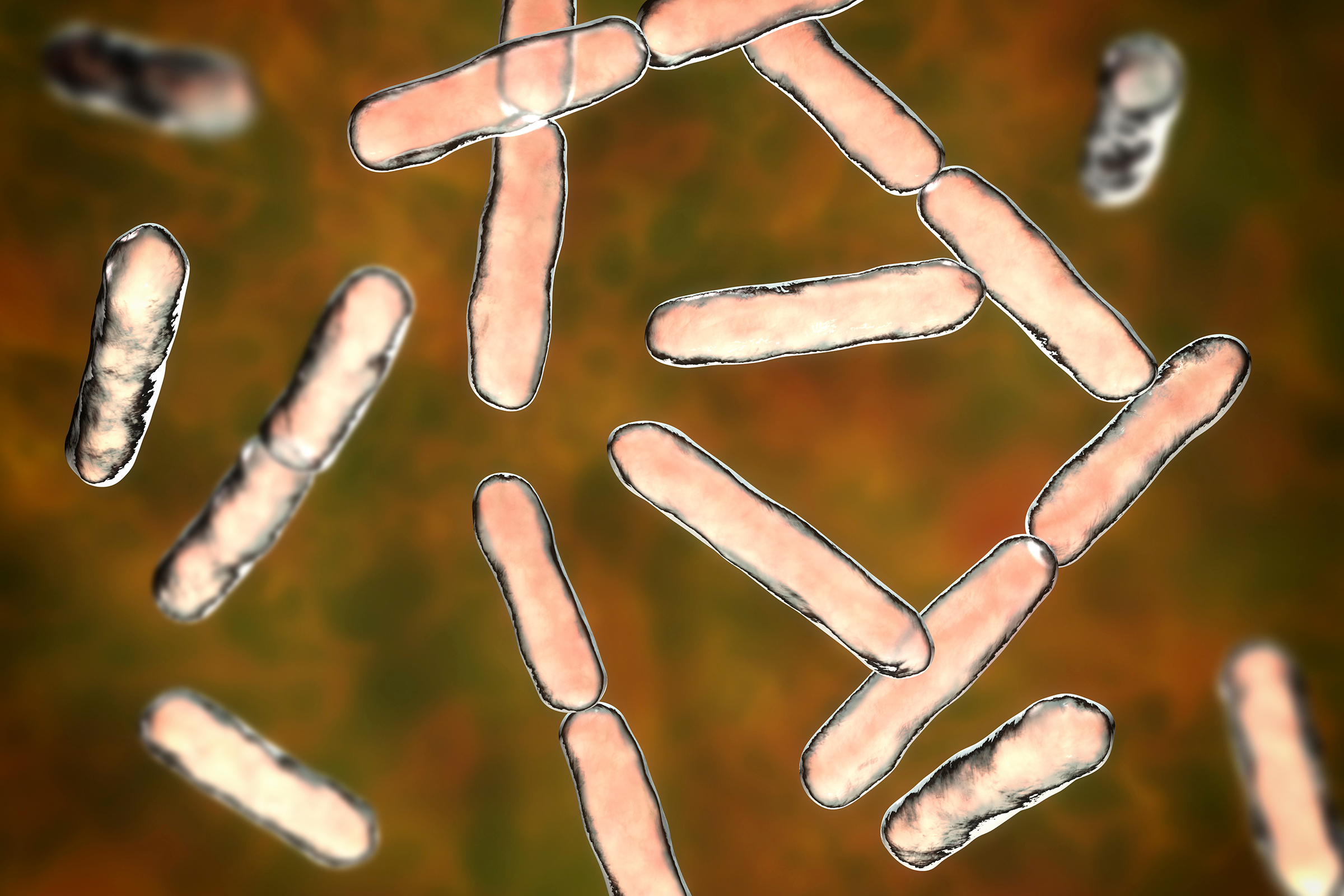
The results showed that babies with higher levels of beneficial bacteria called Bifidobacterium longum, typically acquired through vaginal birth, were less likely to require hospitalization for respiratory infections. These bacteria are known to promote a healthy and stable gut environment, which appears to contribute to stronger immune protection.
However, the researchers found that not all vaginally born babies had these protective bacteria. Those born vaginally without them had similar rates of disease as babies born via cesarean section.
The study reinforces existing evidence about how delivery method affects infant health. Dr. Gina Milone, a maternal-fetal medicine specialist at Stony Brook Medicine who was not involved in the study, noted that babies born vaginally are exposed to their mother’s vaginal microbiome, while those delivered by cesarean section are not.
“This initial exposure to the mother’s microbiome contributes to the development of the infant’s early gut microbiome,” she told The Epoch Times, adding that this microbiome is a critical part of the developing immune system.
The timing of cesarean delivery matters significantly, she noted. “If a patient is in labor or the water bag breaks and they then need to have a cesarean, their baby is still likely exposed to the mother’s vaginal microbiome,” she said.
Babies born via planned cesarean before labor begins—without exposure to the mother’s microbiome—tend to have more difficulty with the initial transition to life outside the uterus and higher rates of respiratory distress compared to those born vaginally.
“If medically possible, vaginal birth is generally safer for both the mother and baby,” Milone said.
What This Means for Future Treatment
Nigel Field, senior study author and professor of infectious disease epidemiology, called the findings “striking and new,” noting they were made possible by the study’s large scale and high-resolution genetic analysis.
However, researchers emphasized that while the study shows a strong association between early gut bacteria and respiratory infection risk, it does not prove that these bacteria directly cause the protection. This may be because the microbiome plays a significant role in the development and maturation of the immune system, including the respiratory immune system.
The team noted that more research—including larger studies—is needed to understand how early gut bacteria influence other health outcomes and to explore ways to support healthy microbiome development in newborns.
“Different types of infant gut bacteria may provide different benefits, and understanding these could pave the way for developing targeted infant probiotics to support early microbiome development,” Trevor Lawley, another senior study author, said in a statement.
He added that, in the future, researchers may be able to develop personalized interventions to optimize a child’s gut microbiome based on their unique microbial profile, potentially supporting better health and development.
How to Reduce a Baby’s Infection Risk
While research continues into microbiome-based therapies, parents can take simple steps to help lower their infant’s risk of infection.
“Hand hygiene and minimizing the contact that your infant has with others who might be carrying a respiratory infection is key,” Milone said.
To help protect a baby during the first weeks:
- Limit early exposure: Allow only close family and friends to visit during the first week. Ask anyone with recent respiratory symptoms to wait until they are fully recovered before meeting the baby.
- Emphasize hygiene: Require all visitors to wash their hands before holding the infant.
- Consider breastfeeding: Provide breastmilk to transfer antibodies, white blood cells, and other immune factors that support immune development. The American Academy of Pediatrics recommends exclusive breastfeeding for about six months. Milone noted that breastfed babies tend to have lower rates of respiratory and other infections.