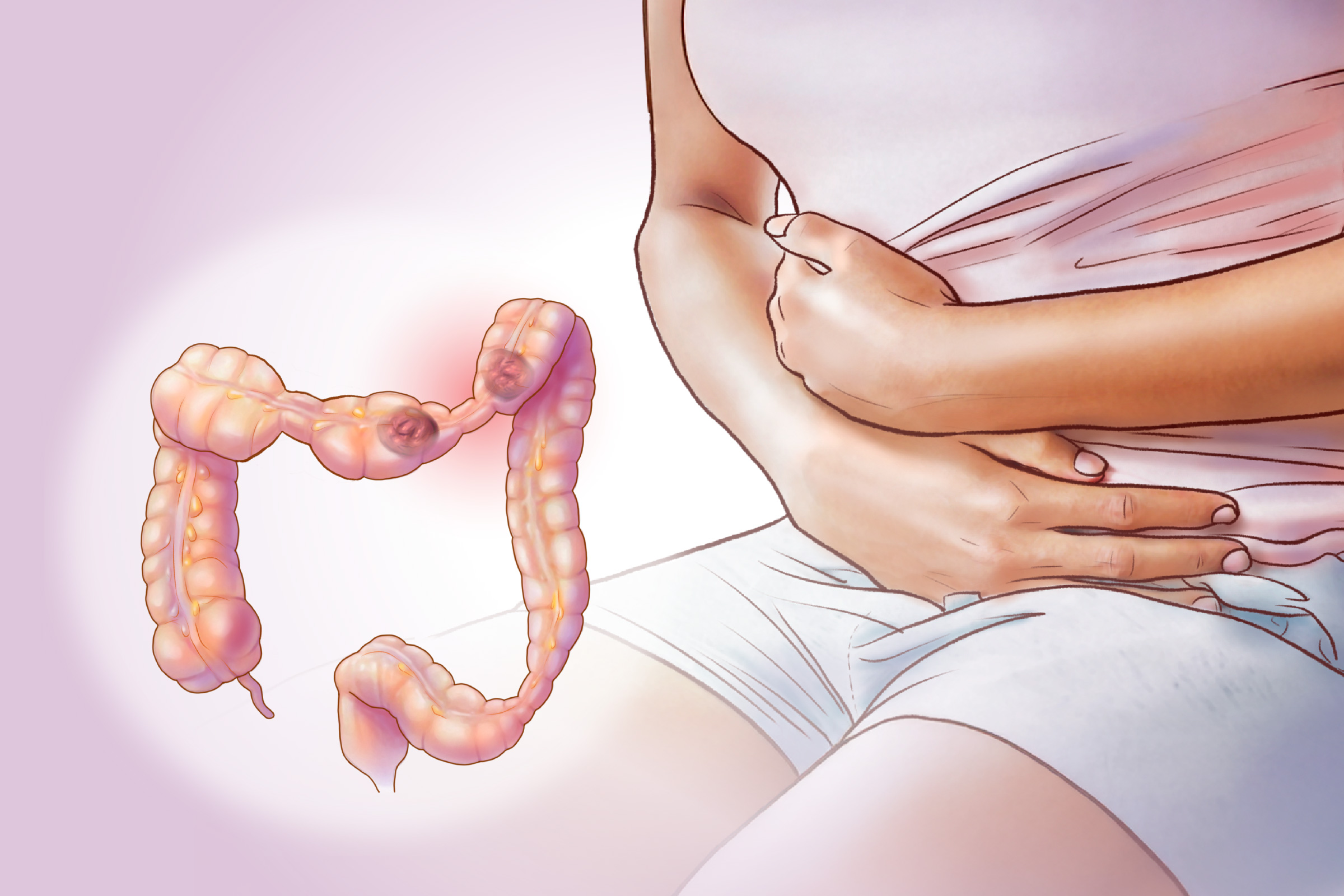
- Abdominal pain or cramping (most common) often occurs after eating and can last for several hours
- Altered stool appearance, mucus in stool, and loose stools
- Changes in bowel movement frequency, including infrequent or difficult movements and sudden urgency to poop
- Excessive gas
- Bloating
- Loss of appetite
IBS often extends beyond digestive symptoms, affecting overall well-being:
- Migraine or recurring headaches
- Difficulty sleeping or disrupted sleep patterns
- Anxiety or depression
- Widespread muscle pain or fibromyalgia
- Persistent pelvic discomfort or chronic pelvic pain
- Urinary issues, such as frequent urination, sudden urges to urinate, or a sensation of incomplete bladder emptying
IBS symptoms can fluctuate, with periods of worsening followed by relief. In some cases, they persist continuously.
The 4 IBS Subtypes
IBS is classified into four subtypes based on whether constipation, diarrhea, or both dominate the symptoms.
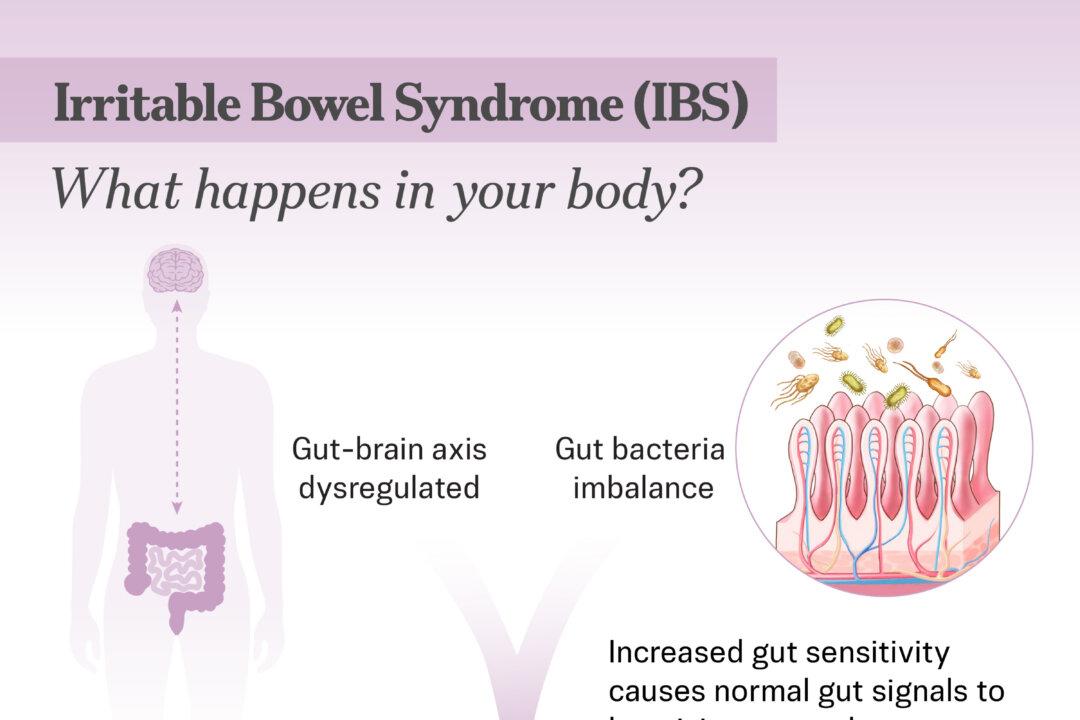
1. Brain-Gut Dysfunction
The gut and brain communicate through a complex network of nerves, hormones, and immune signals called the gut-brain axis. In IBS, this communication becomes dysregulated, making the gut overly sensitive. This causes the brain to misinterpret normal intestinal signals, triggering inappropriate responses such as pain, bloating, and irregular bowel movements.
2. Gut Microbiota Imbalance
Emerging research suggests that imbalances in gut bacteria may play a key role in IBS. The trillions of microorganisms in the digestive tract support digestion, metabolism, and immune function. When this ecosystem becomes disrupted, it can contribute to inflammation and increased gut sensitivity.
3. Food Intolerances or Sensitivities
Up to 90 percent of people with IBS report food intolerances. Certain foods may affect gut movement or interact with the gut microbiome, worsening symptoms. Differences in gut bacteria may also make some people more sensitive to specific foods.
4. Infections
Food poisoning, gastroenteritis, and traveler’s diarrhea can cause long-lasting changes in gut motility and abnormal brain signaling. A 2023 study identified Ruminococcus gnavus as a key bacterial species associated with IBS-D.
5. Early Life Stress
Childhood trauma, abuse, or other stressful experiences can permanently alter the body’s stress-response system, making the gut more sensitive and reactive throughout life.
6. Visceral Hypersensitivity
Overly sensitive nerves in the digestive system cause normal sensations—such as gas or gut movement—to feel painful. This may explain why people with IBS experience discomfort like pain or bloating without an obvious physical issue.
7. Gastrointestinal Dysmotility
Abnormal muscle contractions may cause food to move too quickly, leading to diarrhea (IBS-D), or too slowly, causing constipation (IBS-C).
8. Mucosal Inflammation
In some people with IBS—especially those with diarrhea or a history of gut infection—mild inflammation develops in the intestinal lining. This may include an increase in certain immune cells, which could contribute to ongoing symptoms.
9. Excessive Bile Acids
Normally absorbed in the small intestine, bile acids may reach the colon in excess due to malabsorption. This can lead to diarrhea and cramping.
10. Certain Medications
Antibiotics and some other medications can disrupt the balance of gut bacteria and affect intestinal movement.
11. Small Intestinal Bacterial Overgrowth (SIBO)
SIBO occurs when too many or the wrong types of bacteria grow in the small intestine.
- Sex: IBS occurs nearly twice as often in women as in men, though the reasons remain unclear.
- Family History: Having a parent or sibling with IBS increases the risk of developing it.
- Ultra-Processed Foods: A 2020 study found that people who ate more ultra-processed foods were about 25 percent more likely to develop IBS than those who ate fewer.
- A change in bowel movement frequency
- Pain or discomfort linked to bowel movements
- A change in stool consistency or appearance
Doctors review the patient’s medical history, conduct a physical exam, and run tests to rule out other conditions.
Lab Tests
Lab tests help rule out other conditions that may mimic IBS and provide clues about underlying issues.
- Blood tests to check for anemia, infection, Celiac disease, or inflammation
- Urinalysis to detect urinary tract infections
- Stool tests to identify harmful bacteria, parasites, hidden blood, or inflammatory markers such as calprotectin
- Breath tests to detect bacterial overgrowth
Imaging Tests
The following imaging methods create detailed pictures of internal organs to rule out other causes of IBS symptoms:
- Abdominal X-rays
- CT scans
- MRI
- Ultrasounds
Diagnostic Procedures
Doctors may use upper endoscopy to examine the esophagus, stomach, and upper small intestine, and colonoscopy to evaluate the large intestine for inflammation, ulcers, bleeding, or abnormal growths.
1. IBS Medications
Medications for IBS include both over-the-counter (OTC) and prescription options, tailored to specific symptom patterns.
- OTC therapies for IBS-C: Osmotic laxatives draw water into the colon, bulk-forming laxatives such as psyllium add fiber, and stool softeners help fluids mix into stool.
- Prescription Medications for IBS-C: Gabapentin may relieve nerve pain, while pregabalin can help with IBS-related visceral pain.
- OTC therapies for IBS-D: Antidiarrheal medications such as loperamide can slow down bowel movements.
- Prescription Medications for IBS-D: Bile acid binders such as cholestyramine and colestipol reduce diarrhea; anticholinergic medications such as dicyclomine or hyoscine ease painful spasms; and low-dose tricyclic antidepressants (imipramine, desipramine, or nortriptyline) calm gut nerve signals.
- Alosetron: Relaxes the colon and slows bowel movements. Approved only for women with severe IBS-D who have not responded to other treatments, since its effectiveness in men has not been clearly demonstrated.
- Eluxadoline: Reduces intestinal muscle contractions and fluid secretion, improves rectal muscle tone, and eases diarrhea. Used to treat IBS-D. The drug acts on opioid receptors in the gut but has a low risk of addiction when used as prescribed.
- Rifaximin: An antibiotic used to treat IBS-D, particularly in cases of suspected bacterial overgrowth in the gut, by reducing harmful gut bacteria.
- Lubiprostone: Increases fluid secretion in the small intestine, making it easier to pass stool. Approved only for women with IBS-C who have not improved with other treatments.
- Linaclotide: Promotes fluid secretion in the intestines and helps stool move more easily through the bowel, relieving IBS-C symptoms.
2. Herbal Medicines
Certain herbal preparations may help relieve IBS symptoms, though guidance from a certified herbalist or traditional Chinese medicine practitioner is recommended.
- The Nutrition Care Gut Relief Formula: A 2020 study found that this blend of curcumin, Aloe vera, slippery elm, guar gum, pectin, peppermint oil, and glutamine reduced digestive symptoms by 60 percent to 80 percent in adults with digestive disorders, including IBS. Many participants recovered from intestinal permeability and showed improved gut microbiota, and one-third were able to reintroduce previous food triggers.
- Slippery Elm Formulae: The DA-IBS formula (bilberry, slippery elm, agrimony, and cinnamon) may relieve IBS-D or IBS-M symptoms other than bowel habits. The C-IBS formula (slippery elm, lactulose, oat bran, and licorice root) may improve bowel habits and overall IBS symptoms.
- Turmeric: May improve digestion and regulate bowel movements due to its anti-inflammatory effects. A 2022 systematic review found that medications containing curcumin and turmeric extract may help ease abdominal pain and other IBS symptoms.
- Psyllium Husk: A soluble fiber that absorbs water and adds bulk to the stool, making bowel movements easier. Research shows that it boosts “good” gut bacteria and increases short-chain fatty acids that nourish the gut lining. It also helps regulate stool consistency for both IBS-D and IBS-C, and may reduce gas and bloating when combined with certain fibers, such as inulin.
- Artichoke: Artichoke leaf extract may reduce IBS and indigestion symptoms. A 2004 study found that taking artichoke leaf extract for two months reduced IBS symptoms by 26 percent and indigestion symptoms by 41 percent, and produced a significant shift from alternating constipation and diarrhea to normal bowel movements.
- Peppermint Oil: Menthol, peppermint oil’s active ingredient, relaxes smooth muscles in the gut and reduces nerve sensitivity in the digestive tract, easing abdominal pain, bloating, and discomfort.
- Curcumin and Fennel Essential Oil: Fennel contains anethole, which relaxes gut muscles and relieves cramp-like belly pain. Combined with curcumin, fennel oil may significantly improve IBS symptoms.
3. Physiotherapy
Some people with IBS have pelvic floor muscle incoordination, which makes bowel emptying difficult. A trained pelvic floor physiotherapist can diagnose this through specialized exams. Treatment focuses on teaching the patient to relax the pelvic floor while using deep abdominal muscles to support bowel movements. Physiotherapy may also help with diarrhea-related urgency or incontinence.
4. Acupuncture
Acupuncture has been shown to relieve pain and improve symptoms such as anxiety, migraines, and insomnia associated with IBS.
5. Moxibustion
Acupuncture-moxibustion—a traditional Chinese medicine technique combining acupuncture and heat therapy—has been shown to relieve IBS symptoms with few side effects. Meta-analyses suggest it may work better than some standard Western medications. A 2014 review found that acupuncture-moxibustion may regulate gut movement, sensitivity, brain-gut communication, hormones, and immune function.
6. Osteopathy
Osteopathic manipulative treatment uses hands-on techniques to improve gut function.
7. Therapeutic Massage
Myofascial release, a gentle massage targeting tight areas in muscles and connective tissue, may relieve abdominal pain, bloating, and constipation in adults with IBS. Therapeutic massage may also ease anxiety and promote relaxation.
8. Stress Management (Psychotherapies)
Because stress can trigger or worsen IBS symptoms, stress reduction therapies may be highly beneficial.
- Gut-Directed Hypnotherapy: Uses guided hypnosis and visualization to help patients imagine relief from symptoms. In a study published in April, gut-directed hypnotherapy helped improve overall IBS symptoms—particularly abdominal pain—and group sessions proved effective compared with standard care.
- Fasting Therapy: In one study, 10 days of fasting followed by five days of eating again led to significant improvements in abdominal pain, bloating, diarrhea, nausea, anxiety, and quality of life in IBS patients who had not responded to basic treatment.
- Dynamic Psychotherapy: An intensive talk therapy that addresses emotional causes of symptoms and interpersonal conflicts.
- Cognitive Behavioral Therapy (CBT): A short-term therapy combining various stress management techniques, such as deep breathing, to change how a person responds to anxiety.
- Relaxation Training: Teaches methods to release muscle tension and calm the body.
1. Dietary Strategies
Dietary strategies can help manage IBS symptoms by reducing triggers and supporting healthy digestion.
- Low-FODMAP Diet: Developed by Australian dietitian Sue Shepherd, this diet limits poorly absorbed carbohydrates that can trigger IBS symptoms.
- Fiber: For IBS-C, doctors or dietitians may recommend increasing fiber intake, usually starting with soluble fiber. Insoluble fiber should be added gradually, since it can be harder to tolerate. Insoluble fiber sources include fruits and vegetables with skin, whole grains, and beans. For IBS-D, it’s better to avoid excessive insoluble fiber.
- Fluids: Drinking at least eight to 10 glasses of water daily can help relieve constipation.
- Foods to Eat: To reduce IBS flare-ups, some people may benefit from soy or almond milk, hard cheeses (such as feta), lean protein sources (such as eggs, tofu, poultry, and seafood), and well-tolerated vegetables (such as carrots, tomatoes, lettuce, potatoes, and zucchini).
Certain herbs and foods may help with different symptoms: ginger may reduce inflammation and intestinal sensitivity associated with IBS-D, chamomile may ease stomachaches with its anti-inflammatory and muscle-relaxing effects, dried plums or prunes may relieve IBS-C because of their fiber content and natural laxative properties, and eating oats and up to one tablespoon of whole or ground flaxseeds daily may help ease bloating and gas. - Foods and Beverages to Avoid: Limit or avoid alcohol, caffeine, gas-producing foods (such as beans, cabbage, cauliflower, broccoli, Brussels sprouts, onions, and apple), high-sugar items (such as soda and candy), sugar alcohols found in sugar-free products (such as sugar-free gums), and high-fat foods.
Some people may also need to avoid gluten (a protein in wheat, barley, and rye) and lactose-containing dairy if these worsens their symptoms.
2. Dietary Supplements
Several nutritional and microbial supplements may help relieve IBS symptoms.
- Probiotics: These “good bacteria” may help reduce IBS symptoms. Because probiotics come in capsules, liquids, powders, and gummies, finding the most effective type may require some trial and error.
- Vitamin D: May reduce IBS symptom severity, particularly in people with a deficiency or insufficiency.
- Magnesium: Magnesium oxide has been widely used in Japan to treat constipation. A 2019 study found that patients with mild to moderate constipation experienced more spontaneous bowel movements and less constipation compared with placebo.
- Melatonin: May ease abdominal pain, regulate gut motility, and improve stress and mood disturbances. Melatonin may reduce IBS symptoms whether or not patients have sleep problems.
- Digestive Enzymes: Although IBS is not caused by the lack of digestive enzymes, supplements such as lipase, protease, amylase, and lactase may help break down food components and ease symptoms.
3. Low-Impact Exercises
Regular, gentle exercise for at least 30 minutes each day may reduce anxiety, improve gut health, and ease IBS symptoms. A few good options include:
Aerobic exercise: Stimulates the muscles in the intestines, helping them move food waste more efficiently.
Walking: Short walks before breakfast or after dinner may help. Start with five to 10 minutes and gradually build up to 30 minutes.
4. Forest Bathing and Nature Walks
Forest bathing (known as Shinrin Yoku in Japan) and walking in nature have been shown to lower cortisol (a stress hormone), promote relaxation, and activate the parasympathetic nervous system (responsible for rest and digest), which supports healthy digestion. Nature exposure can also improve sleep and reduce anxiety, both of which positively influence the gut-brain axis.
5. Self-Massage
Self-massage may help relieve abdominal discomfort. While lying down, gently massage your abdomen in a clockwise direction using one hand.
6. Mindfulness Meditation
Mindfulness meditation is a psychological approach that helps manage IBS by focusing on mind-body connections and self-regulation. It has been shown to reduce both stress and pain, making it a promising approach for IBS symptom relief.
7. Quality Sleep
Many people with IBS experience sleep disturbances. Improving sleep habits may reduce anxiety and digestive symptoms. A 2023 study found that people who perceived their sleep as poor had worse gut symptoms the next day, regardless of actual sleep quality.
8. Music Therapy
Music therapy may reduce anxiety and diarrhea in people with IBS, improving quality of life. One approach, the Bonny Method of Guided Imagery and Music, uses classical music and guided imagery to promote emotional healing. This method has shown positive results in regulating stress responses that often trigger or worsen IBS symptoms.
Comorbid Conditions
People with IBS may also experience several overlapping conditions.
- Sleep Disturbances: Difficulty falling asleep, staying asleep, or achieving restful sleep
- Fibromyalgia: Widespread muscle pain, fatigue, and increased sensitivity to touch
- Back Pain: Ongoing discomfort or pain in the back
- Chronic Pelvic Pain: Persistent lower abdominal or pelvic pain lasting six months or longer
- Interstitial Cystitis: Bladder pressure, pain, and frequent or urgent urination
- Temporomandibular Joint Disorder: Dysfunction or pain in the jaw joint and surrounding muscles, affecting chewing and speaking
- Gastroesophageal Reflux Disease: Stomach acid flowing back into the esophagus, causing heartburn or acid regurgitation
- Post-Traumatic Stress Disorder: Flashbacks, anxiety, and avoidance linked to a traumatic event
IBS is not linked to Crohn’s disease, ulcerative colitis, or other inflammatory bowel diseases. However, people with these conditions may also experience IBS-like symptoms.
General Complications
Complications are infrequent but may affect quality of life across IBS subtypes.
Mood disorders: Anxiety or depression that may worsen IBS symptoms
Poor Quality of Life: Moderate to severe IBS may impair daily functioning and reduce work performance
Complications associated with IBS-C:
- Hemorrhoids: Swollen blood vessels in the rectum or anus that may cause bleeding, discomfort, or protrusion during bowel movements
- Anal Fissure: A small tear in the anal lining, often from passing large or hard stools, causing pain and bleeding
- Fecal Impaction: A compacted mass of stool in the rectum that cannot be passed naturally and may require manual removal
- Rectal Prolapse: Rectal tissue slipping or protruding through the anus, often due to straining
- Lazy Bowel Syndrome: Dependence on laxatives for bowel function, typically from overuse
Complications associated with IBS-D:
Nutritional Deficiencies: Over-restricting foods may lead to nutrient deficiencies and potential health issues
Dehydration: Frequent diarrhea can cause fluid and electrolyte loss, leading to dehydration or electrolyte abnormalities if not properly managed