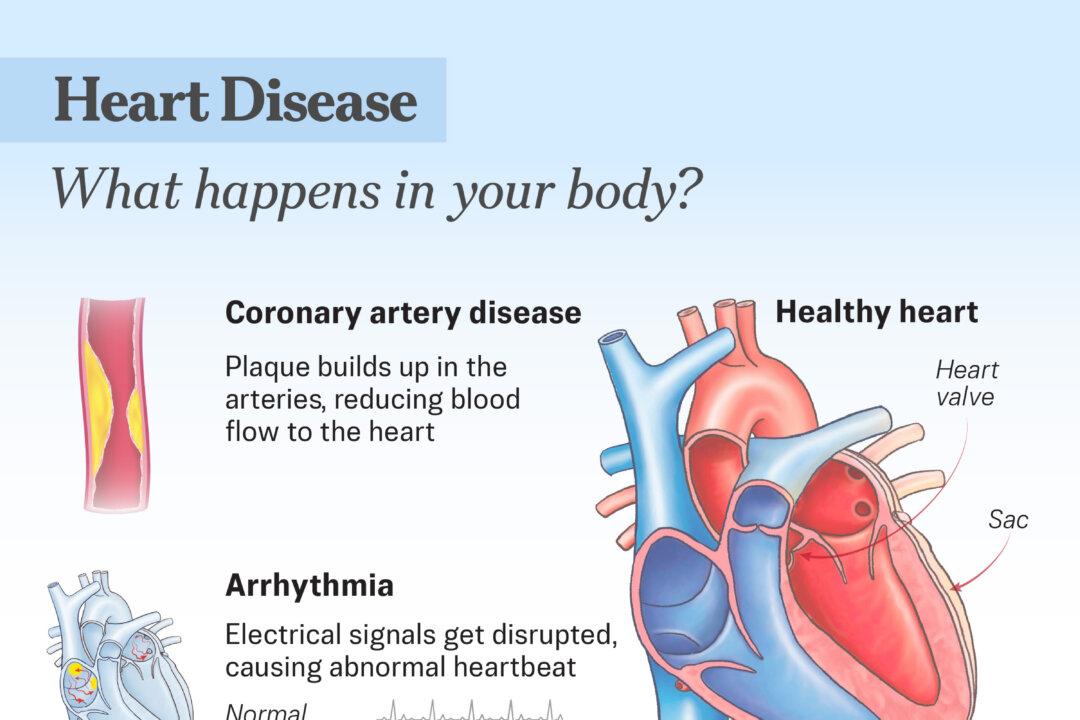
Coronary Artery Disease
Affecting around 5 percent of American adults aged 20 and older, it is the most common type of heart disease. It develops when plaques—made up of fat, cholesterol, and other substances—build up in the arteries. If a plaque ruptures, the body forms a blood clot to repair it, which can block the arteries supplying oxygen-rich blood to the heart muscle and trigger a heart attack or cardiac arrest.
Arrhythmias
Heart rhythm disorders occur when the heart beats too fast, too slow, or irregularly. The heart’s rhythm is controlled by electrical signals that coordinate how quickly and regularly it beats. When these signals are disrupted—either because the nerve cells that produce them malfunction, the signals do not travel properly, or another part of the heart starts sending competing signals—an irregular heartbeat can occur. Certain arrhythmias can be serious or even life-threatening, such as atrial fibrillation.
Cardiomyopathy
A disorder of the heart muscle that causes it to enlarge or stretch, reducing the heart’s ability to pump blood effectively and sometimes leading to abnormal heart rhythms.
Heart Valve Disease
Occurs when one or more heart valves do not open or close properly. It can be congenital or acquired later in life, and its exact cause is not always known.
Myocarditis and Pericarditis
Myocarditis occurs when the heart muscle becomes inflamed, while pericarditis is inflammation of the thin, protective sac surrounding the heart. These conditions can be caused by viruses, bacteria, fungi, or parasites. Viruses are the most common cause. They can infect the heart muscle and trigger an immune response that leads to inflammation.
Lifestyle Risk Factors
These factors are largely manageable and present an opportunity for risk reduction.
- Unhealthy Diet: A diet high in refined carbohydrates, unhealthy fats, and salt can contribute to increased cholesterol levels and elevated blood pressure.
- Sugary Drinks: A January study found that drinking sugary beverages may be connected to about 1 in 10 new Type 2 diabetes cases and 1 in 30 new cardiovascular disease cases.
- Insufficient Physical Activity: Lack of regular exercise can increase the likelihood of high blood pressure, high cholesterol, and excess body weight—all of which are risk factors.
- Excess Body Weight: Increases the likelihood of developing diabetes and high blood pressure.
- High Levels of Stress: Are linked to an increased risk of cardiovascular events in people with a history of social isolation, childhood abuse, or trauma. Stress activates brain regions such as the amygdala, setting off hormonal and immune reactions that raise blood pressure, cause inflammation, and speed up plaque buildup in arteries—factors that can lead to heart attacks and other heart problems.
- Type A Personality: Is characterized by high levels of competitiveness, urgency, and hostility, often combined with a strong drive to achieve. The Type A behavior pattern was first described in the 1950s by cardiologists Meyer Friedman and Ray Rosenman, who suggested that it could be a significant risk factor for coronary heart disease. Free-floating hostility—easily triggered anger—is a key feature of the Type A behavior pattern, and anger and hostility are linked to coronary artery disease, heart attacks, arrhythmias, and an increased risk of sudden cardiac death.
- Tobacco Use: Is a major risk factor, as smoking and vaping can damage and constrict blood vessels.
- Heavy Alcohol Intake: Can raise cholesterol and blood pressure levels and lead to weight gain.
- Illegal Drug Use: Negatively affects the cardiovascular system, causing issues from irregular heartbeats to heart attacks.
- Artificial Light: Exposure at night to artificial light disrupts the body’s natural circadian rhythms—mainly by suppressing melatonin secretion—which can increase heart rate, inflammation, insulin resistance, and artery plaque buildup. This disruption can ultimately raise the long-term risk of cardiovascular diseases such as heart attack, heart failure, and atrial fibrillation.
- Air Pollution: Long-term exposure to air pollution is associated with a higher risk of stroke and coronary heart disease.
- COVID-19 Vaccines: Myocarditis and pericarditis are recognized as rare yet serious side effects of COVID-19 vaccination. A 2023 study found that myocarditis can sometimes occur within a week after receiving mRNA COVID-19 vaccines, especially in men under 40. According to an October study, most pericarditis cases are mild and resolve on their own, but some people experience recurrent or hard-to-treat inflammation that requires longer-term care.
Medical Conditions
Several medical conditions can contribute to the risk of heart disease. While not entirely controllable, many can be managed with proper medical care.
- High Blood Pressure: Is a major risk factor for cardiovascular disease; when elevated, it can damage blood vessels.
- High Cholesterol: Can narrow blood vessels and raise the risk of blood clots.
- Diabetes: Raises blood sugar levels, which can damage and narrow blood vessels. It also often occurs alongside excess body weight.
- Sleep Apnea: Increases the risk of heart failure by 58 percent and coronary heart disease by 30 percent.
- Chronic Kidney Disease: Reduces kidney function and shares many risk factors with heart disease. It can also cause hypertension, which in turn raises cardiovascular risk.
- Metabolic Syndrome: Is a cluster of conditions—including high blood pressure, high blood sugar, unhealthy cholesterol levels, and abdominal obesity—that collectively damage blood vessels and cause plaque buildup and inflammation.
- Certain Pregnancy Conditions: Include preeclampsia, or high blood pressure during pregnancy, and gestational diabetes, which can strongly indicate a higher future risk of heart disease.
- Chest Pain: Is the most common symptom of reduced blood flow to the heart or a heart attack. The pain can vary in type and intensity—from mild discomfort to crushing, squeezing, or burning sensations—and does not always reflect the severity of the heart problem.
- Shortness of Breath: Occurs when the heart cannot pump blood effectively, causing fluid buildup in the lungs. It is a common symptom of heart failure and arrhythmias and can happen during activity, at rest, or when lying flat.
- Palpitations: Refer to a fast or uneven heartbeat that can occur when the heart struggles to pump blood effectively or as a common sign of an arrhythmia, although palpitations appear in other types of heart disease as well.
- Persistent Coughing or Wheezing: May indicate fluid buildup in the lungs—a possible sign of heart problems. In some cases, the person may cough up pink or bloody mucus.
- Edema (Swelling): Occurs when the heart’s function is reduced, causing blood flow to slow and back up in the veins. This leads to a fluid buildup and swelling in the legs, ankles, or feet. Swelling may also occur in the abdomen, and may sometimes be accompanied by weight gain.
- Unusual Fatigue: Involves feeling unusually tired or suddenly weak, or being so exhausted that normal daily activities become difficult.
- Poor Blood Supply to the Extremities: Is caused by the narrowing of the arteries from plaque buildup. While this is not heart disease, it increases the risk of a heart attack. It can cause pain, fatigue, burning, or discomfort in the legs—especially during activity—as well as numbness, coolness, or pale skin at rest.
Heart Attack
A heart attack happens when blood flow to part of the heart is suddenly blocked, cutting off oxygen and damaging the heart muscle. Getting help fast is critical—the sooner treatment begins, the better the chances of recovery.
- Chest Discomfort: Most heart attacks cause discomfort in the center of the chest that lasts several minutes or comes and goes. It may feel like pressure, squeezing, fullness, or pain.
- Upper Body Discomfort: Pain or discomfort can also occur in the arms, back, neck, jaw, or stomach.
- Shortness of Breath: Trouble breathing may happen with or without chest discomfort.
- Other Signs: Symptoms such as cold sweats, nausea, a fast or irregular heartbeat, unusual tiredness, or lightheadedness may also occur.
Cardiac Arrest
Cardiac arrest is different from a heart attack. It occurs when the heart’s electrical system malfunctions, causing the heart to stop beating suddenly. Without immediate emergency care, it can be fatal within minutes. If you notice anyone showing the following signs, call 911 immediately:
- Sudden Loss of Consciousness: The person does not respond when you tap their shoulders or try to get their attention.
- Abnormal Breathing: The person does not breathe normally when you tilt their head back and watch for at least five seconds.
- Electrocardiogram (ECG or EKG): A quick, painless test that records the heart’s electrical signals to detect abnormal heart rhythms.
- Holter Monitoring: A wearable device that records heart activity over a day or more to detect irregular rhythms that a standard ECG might miss.
- Echocardiogram: A diagnostic test that uses sound waves to create moving images of the heart, showing how blood flows and how well the valves function.
- Exercise Stress Tests: A test that monitors the heart’s response to physical exertion—typically on a treadmill or stationary bike—or uses medication to simulate exercise if physical activity is not possible.
- BNP Blood Test: A blood test that measures the hormone B-type natriuretic peptide, which helps assess the severity and prognosis of heart failure.
- Cardiac Catheterization: A procedure that involves inserting a thin, flexible tube known as a catheter into a blood vessel to inject dye and visualize artery blockages in the heart.
- Imaging Tests: Diagnostic tests that include cardiac CT and MRI scans, or a chest X-ray to provide detailed images of the heart’s structure and function.
1. Medications
Medications are often the first line of treatment for managing heart disease. They help control symptoms, prevent complications, and improve long-term outcomes.
- Heart and Blood Pressure Relief: Medications such as beta blockers and ACE inhibitors lower blood pressure and decrease the heart’s workload.
- Chest Pain (Angina) Relief: Medications such as nitrates and other medicines are used to ease or prevent chest pain.
- Cholesterol-Lowering Medicines: Medications such as statins control high cholesterol and slow plaque buildup. Nonstatins such as ezetimibe, bile acid sequestrants, and PCSK9 inhibitors may be used when statins are insufficient or not tolerated. Drugs that lower triglycerides, including fibrates, omega-3s, and niacin, may also be used.
- Blood Thinners: Medications such as low-dose aspirin and dual-antiplatelet therapy help prevent dangerous blood clots, especially in people who have had a heart attack or a stent placed.
- Anti-Inflammatory: Medications such as colchicine may be prescribed to control inflammation associated with coronary heart disease.
Arrhythmias
- Antiarrhythmics: A class of medications that help control abnormal heart rhythms. Examples include beta blockers, potassium channel blockers, calcium channel blockers, and amiodarone.
- Anticoagulants: A class of drugs that help prevent blood clots in people with arrhythmias. Examples include warfarin, dabigatran, rivaroxaban, apixaban, and edoxaban.
- Digoxin: A cardiac glycoside that helps the heart pump more strongly, slows the heart rate, and can reduce fatigue and shortness of breath.
Cardiomyopathy
- ACE inhibitors or angiotensin receptor blockers
- Beta blockers
- Calcium channel blockers
- Antiarrhythmic drugs
- Anticoagulants
- Digoxin
Heart Valve Disease
- Diuretics to reduce fluid buildup
- Blood thinners to prevent clots and related complications
- Antiarrhythmics to manage abnormal or rapid heartbeats
Myocarditis
- ACE inhibitors or ARBs to lower blood pressure and support heart muscle recovery
- Beta blockers to control arrhythmias and aid in heart remodeling
- Diuretics to reduce fluid buildup caused by heart weakness
In certain inflammatory cases, corticosteroids may be used to decrease inflammation.
2. Surgeries
When medications alone are not enough, surgery may be necessary to restore heart function or correct structural problems.
- Bypassing Blocked Arteries: A major surgery, also called coronary artery bypass grafting, that uses a healthy blood vessel from another part of the body to create a new route for blood flow and bypass a severely blocked coronary artery.
- Other Procedures: Less common procedures—such as transmyocardial laser revascularization and coronary endarterectomy—may be used to relieve severe chest pain when standard treatments are too risky or ineffective.
Arrhythmias
- Ablation: The destruction of small areas of heart tissue that cause arrhythmias.
- Cardioversion: A procedure used to stop irregular heartbeats and restore normal rhythm.
- Implantable Devices: Devices such as pacemakers and implantable cardioverter defibrillators that regulate or shock the heart back to a normal rhythm.
- Left Atrial Appendage Closure: A procedure that reduces stroke risk by sealing off a small pouch in the heart where blood clots can form.
Cardiomyopathy
- Septal Ablation: A procedure that involves injecting alcohol through a catheter to shrink thickened heart muscle and improve blood flow in people with hypertrophic cardiomyopathy.
- Radiofrequency Ablation: A procedure that uses a catheter to deliver heat energy that destroys small areas of abnormal heart tissue responsible for irregular heart rhythms. In severe cases where heart failure progresses despite medications and other treatments, a heart transplant may be considered as a last-resort option to replace the failing heart and restore normal function.
Heart Valve Disease
- Valve Replacement: A procedure that removes and replaces the damaged valve with a mechanical or biological one.
- Annuloplasty: A procedure that repairs an enlarged valve ring by tightening it with sutures or a supporting device.
Myocarditis
3. Nonsurgical Procedures
Nonsurgical interventions can often restore normal heart function without the need for open-heart surgery.
- Balloon Valvuloplasty: A minimally invasive procedure that uses an inflated catheter balloon to widen narrowed valves and improve blood flow.
- Transcatheter Valve Replacement: A minimally invasive procedure that involves implanting artificial valves made of metal or synthetic materials. These valves are durable and often used in younger patients, but require lifelong blood thinners to prevent clots and strokes. Bioprosthetic valves, made from animal tissue, generally don’t require long-term blood thinners.
Pericarditis
In rare cases, inflammation around the heart can cause fluid to accumulate inside the protective sac, creating dangerous pressure that limits the heart’s ability to pump. When this happens, quick medical intervention is essential. Pericardiocentesis is a procedure used in such situations, especially when pericarditis leads to significant fluid buildup. In this procedure, a needle or catheter is inserted through the chest wall to drain the excess fluid from the pericardium, relieving pressure and restoring normal heart function. This helps prevent serious complications like cardiac tamponade, a life-threatening condition that occurs when the pressure on the heart becomes dangerously severe.
4. Herbal Remedies
Always consult a qualified health care provider or licensed herbalist before using herbal remedies for heart conditions.
- Guggul: A natural resin from the Commiphora mukul tree, used for thousands of years to help manage conditions such as high cholesterol and hardening of the arteries. Its main active ingredient, called guggulsterone, may support heart health by lowering cholesterol, reducing inflammation, and acting as an antioxidant. In one study of 200 people with heart disease and chest pain, five months of guggul treatment led to significant improvements in heart health. Cholesterol, triglycerides, and total blood fats dropped significantly, and about one-quarter of participants no longer had chest pain, while the rest reported less pain.
- Arjuna: A tree whose bark has long been used in traditional Indian medicine to help with chest pain, high blood pressure, and heart failure. Research suggests it may protect the heart by improving blood flow, lowering cholesterol, and preventing artery blockage. Its natural compounds—especially triterpenoids and flavonoids—act as antioxidants that help reduce heart damage.
We’ll introduce more food-grade herbs in the following section.
5. Acupuncture
Acupuncture may benefit cardiovascular health by influencing the nervous and hormonal systems that regulate heart and blood vessel function. Research suggests that acupuncture can help regulate blood pressure, improve circulation, and reduce inflammation by stimulating the release of neurotransmitters and hormones that influence cardiovascular function.
1. Wearable Devices
Research increasingly supports the use of wearable devices—including smartwatches, rings and wristbands—to assess cardiovascular risk and aid in the prevention, diagnosis, and management of heart disease.
2. Meditation
Meditation and mindfulness practices may support cardiovascular health by reducing stress, improving blood pressure, and regulating inflammation.
3. Regular Exercise
Exercise is one of the most effective ways to strengthen the heart and improve circulation. It boosts blood flow, delivers more oxygen to cells, and regulates hormones and blood sugar. Research shows that regular exercise can be as effective as certain medications in preventing coronary heart disease and supporting heart failure recovery.
4. Supplements
Certain nutritional supplements may help support cardiovascular function and reduce risk factors for heart disease. Always talk with a health care provider before adding supplements to your routine.
- Coenzyme Q10 (CoQ10): A vitamin-like substance present in every cell that helps protect the heart and muscles. For people with heart failure, CoQ10 supplements may improve heart function and potentially reduce the risk of cardiovascular death.
- Red Yeast Rice: A natural product that contains monacolin K, a compound that can help lower triglycerides, total cholesterol, and “bad” low-density lipoprotein cholesterol. A study published this year found that red yeast rice may be a promising daily option for managing high cholesterol without the side effects associated with statins.
- Iron: A mineral essential for oxygen transport and energy production in the body. A March study found that iron deficiency in heart attack patients was linked to poorer outcomes, including lower physical capacity and higher chances of rehospitalization. Supplementing iron may help improve heart healing and function in patients with iron deficiency after a heart attack.
- Capsaicin: A natural compound that gives chilli peppers their heat and may help protect the heart by improving exercise tolerance in angina, slowing atherosclerosis, lowering blood pressure and blood sugar, reducing heart muscle thickening, supporting weight management, and decreasing the risk of metabolic syndrome.
- Omega-3s: A group of essential fatty acids that help reduce the risk of cardiovascular events such as heart attacks and strokes in people with heart disease.
5. Music
Music can be a simple yet powerful tool for supporting heart health. Listening, singing, or engaging with music can reduce stress and improve circulation.
6. Plant-Based Products
Several plant-derived compounds have shown promise for supporting cardiovascular health through their anti-inflammatory, antioxidant, and cholesterol-lowering effects.
- Berberine: A plant compound that offers multiple health benefits, including improved cognitive function, blood sugar control, and immune support. A 2023 meta-analysis of 44 studies found that berberine improved blood lipids, reduced inflammation, and slowed atherosclerosis with minimal risks—and in some cases, outperformed statins in lowering stroke risk and arterial plaque buildup.
- Natto: A traditional fermented soybean dish containing nattokinase, an enzyme that may help manage atherosclerosis and lipid levels. A 2017 study reported that nattokinase reduced plaque buildup by 36.6 percent, compared to 11.5 percent among those taking statins.
- Bergamot: A citrus fruit known for its anti-inflammatory and antioxidant properties that may help protect the heart by improving cholesterol balance. In a 2016 study of 80 people with high cholesterol, six months of bergamot supplementation significantly reduced small, dense low-density lipoprotein particles linked to higher cardiovascular risk.
- Hawthorn: A flowering plant whose extracts may protect the heart by lowering cholesterol, reducing inflammation, and fighting oxidative damage. They may also help keep blood vessels healthy. A 2024 study found that a specialized hawthorn extract may help support heart rhythm and overall heart function.
- Garlic: A common culinary plant known to support heart health by lowering blood pressure and cholesterol and improving artery function. A 2023 systematic review and meta-analysis found that garlic significantly raised high-density lipoprotein or “good” cholesterol, lowered low-density lipoprotein or “bad” cholesterol, reduced inflammation, and decreased coronary calcification in people with coronary artery disease. It was considered a safe, natural intervention for reducing key cardiovascular risk factors.
1. Monitor Your Health
- Get regular cholesterol and blood pressure checks to detect problems early.
- Manage chronic conditions such as diabetes or kidney disease with your doctor.
2. Quit Harmful Substances
- Stop smoking and avoid recreational drugs entirely. Quitting lowers your risk quickly, as tobacco damages blood vessels and strains the heart.
- Limit alcohol to no more than two drinks per day for men and one drink for women, as excessive drinking raises cholesterol and blood pressure.
3. Stay Active
Aim for 30 to 60 minutes of physical activity each day to control weight and reduce risk factors such as high blood pressure, diabetes, and high cholesterol.
4. Eat a Heart-Healthy Diet
Focus on nutrient-rich whole foods that help lower inflammation, blood pressure, and unhealthy cholesterol:
- Colorful vegetables and fruits
- Herbs, spices, and teas
- Legumes, nuts, and seeds
- Wild-caught fish
- Healthy fats such as olive oil and avocados
- Dark chocolate (moderate intake is linked to a decreased risk of heart disease)
Limit salt, sugar, processed carbohydrates, and saturated fats.
5. Maintain a Healthy Weight
Keep your weight within a moderate range to reduce strain on the cardiovascular system.
6. Prioritize Sleep
Aim for at least seven hours of sleep each night to lower the risk of high blood pressure, obesity, diabetes, and heart attack.
7. Manage Stress Effectively
Use healthy coping methods such as meditation, exercise, and relaxation techniques rather than turning to unhealthy habits. Even taking a few minutes daily to unwind can make a difference.
8. Consider Nutritional Supplements
Maintain healthy nutrient levels to support cardiovascular function, especially with age. Consult your health care provider to determine which supplements may be appropriate for your needs.
- Sudden Cardiac Arrest: The heart suddenly stops beating because of an unexpected electrical problem, creating a medical emergency.
- Aneurysm: A weakened, bulging section of an artery that can burst, causing dangerous internal bleeding.
- Cardiogenic Shock: A rare but critical condition in which the heart suddenly fails to pump enough blood to support the body’s organs.
- Blood Clots: A buildup of clotted blood in the heart that can occur when blood is not pumped efficiently, increasing the risk of stroke or embolism.