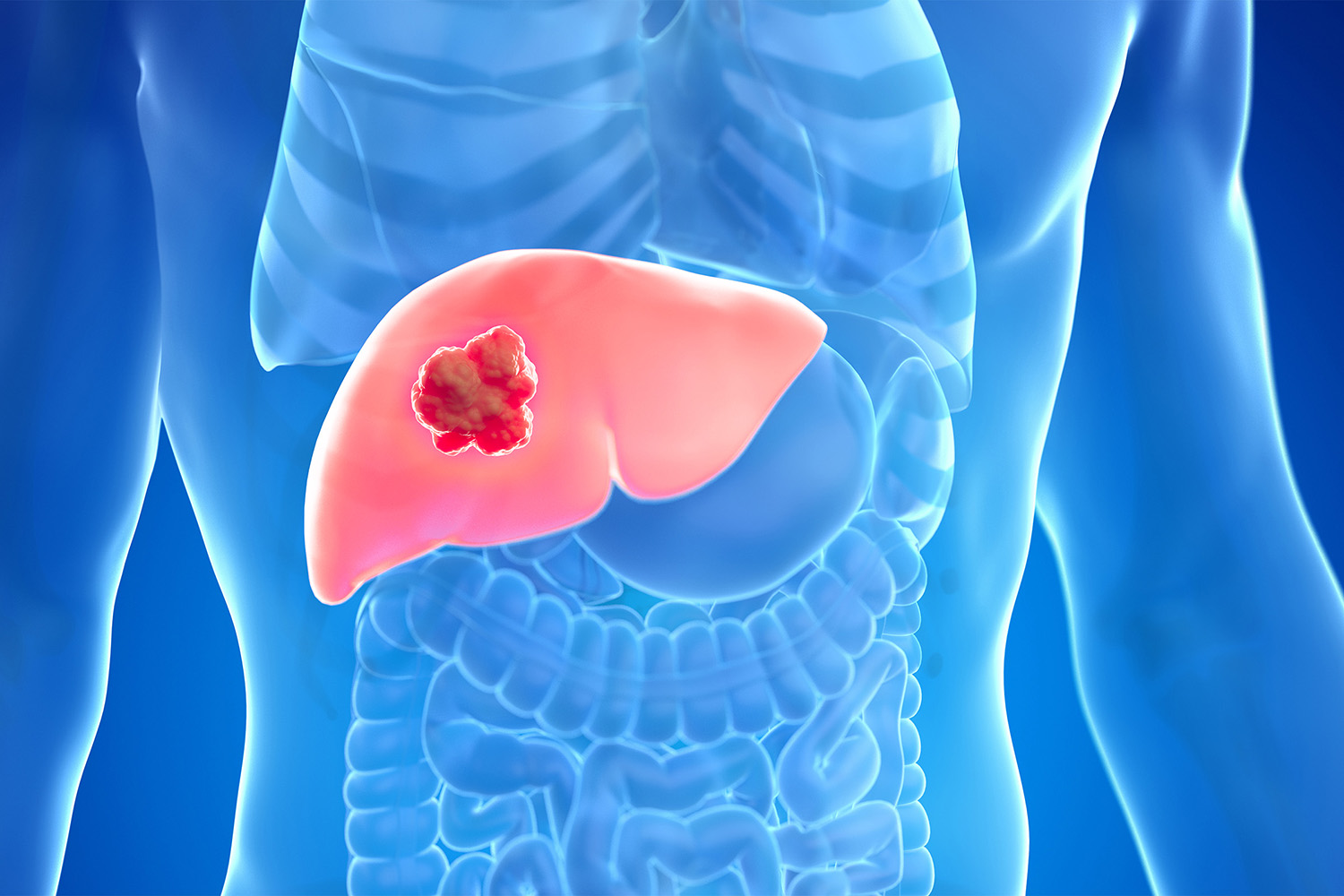
Liver cancer rates are climbing fast.
As fast food chains, supersized sodas, sedentary lifestyles, and chronic infections have become more prevalent over the past 50 years, liver cancer has become increasingly linked to everyday choices.
The bright side is that up to 60 percent of cases could be prevented by addressing key risks.
The Drivers of Liver Cancer
About 870,000 people worldwide are living with liver cancer, and that number could nearly double by 2050.
“Alcohol is considered the single biggest risk factor for liver cancer,” Aleksandra Olsen, communications officer at the World Health Organization Regional Office for Europe, told The Epoch Times.
Not only can alcohol initiate the cancer cells’ development, but it can also speed tumor growth. That’s because alcohol and its byproduct, acetaldehyde, harm the liver in several ways. This combination creates oxidative stress, a kind of internal rusting, that damages DNA and makes it harder for cells to repair themselves, thus contributing to cancer development. Repeated injury from alcohol leads to scarring or cirrhosis, which is where most alcohol-related liver cancers begin.
Alcohol makes the body more vulnerable to other cancer-causing substances, such as tobacco. It also disrupts one-carbon metabolism, a system that helps control which genes are switched on or off. When this process goes wrong, protective genes may be silenced while harmful ones become active.
However, liver cancer can be caused by more than just alcohol. What we eat also matters. Diet can either protect the liver or contribute to the buildup of fat and disease.
Excess fat around the belly can put stress on the liver, while an imbalanced gut microbiome can exacerbate the stress. High-fructose diets, for example, can alter the gut microbiome in unhealthy ways, disrupting the balance between two major bacterial groups, Firmicutes and Bacteroidetes, a change associated with metabolic syndrome. Over time, this pathology can raise the risk of fatty liver disease and even liver cancer.
This applies only to industrial sources of fructose, such as high-fructose corn syrup in soda and processed foods, not to fruit. The processed form of fructose is strongly linked to liver scarring or fibrosis because it is processed by the liver and drains the liver’s energy supply, making it harder for liver cells to function properly.
Another driver of liver cancer is chronic viral infection with hepatitis B or C. When these viruses infect the liver, they disrupt the normal control of cell growth to ensure their own survival. At the same time, the immune system’s attempt to fight the infection adds more stress and damage. Together, the viruses and the body’s response to them create conditions in which liver cancer can take hold.
Prevention–Better Than Cure
Prevention matters because liver cancer doesn’t happen all at once. It usually develops slowly, starting with long-term liver problems, then moving to scarring and cirrhosis, and finally cancer. This lengthy process gives doctors and patients plenty of opportunity to step in with medical treatments and lifestyle modifications to stop the disease before it develops too far.
Reducing Alcohol
Public health policies can help shape lifestyle choices, Dr. Frank Murray, a hepatologist, told The Epoch Times.
At the individual level, however, support and open conversations matter. People who want to cut back on alcohol often need a nonjudgmental space to talk about their drinking and the risks that come with it.
The first step is recognizing that alcohol has become a problem. From there, it can help to set safe, realistic goals—such as drinking less often, avoiding certain triggers, or swapping drinking alcohol for healthier activities, Murray said.
“Even small changes, like choosing nonalcoholic options or avoiding drinking in rounds, can make a real difference,” he said.
Olsen also suggested a few practical strategies for anyone trying to reduce their drinking:
- Know Your Limits: Track how much you drink in a week, set limits, and check in regularly.
- Set Personal Goals: Decide ahead of time how many drinks you’ll have and stick to it. Build in alcohol-free days or weeks if you drink daily.
- Eat and Hydrate: Drink water and eat before or while drinking—this can reduce both thirst and alcohol absorption.
Diet and Important Nutrients
A healthy diet is key to helping
reduce fat in the liver and protect it from metabolic damage. The Mediterranean diet—rich in fruits, vegetables, whole grains, and healthy fats—has been shown to improve liver and metabolic health, primarily because of its high antioxidant content.
Low-carb diets can also help by improving insulin sensitivity, as excess carbohydrates—especially those in high-fructose foods and sugary drinks—can quickly be converted into fat in the liver.
The type of fat you eat matters, too. Omega-3 fats—found in fatty fish such as salmon and sardines, as well as in flaxseeds, chia seeds, and walnuts—are beneficial for liver function, reducing inflammation and scarring, and helping the liver to burn fat instead of storing it.
Some supplements may also help:
- Vitamin E: About 800 IU per day may reduce fat buildup in the liver.
- Silymarin: Extracted from milk thistle seeds, silymarin has been shown to lower liver enzymes and blood fats, supporting overall liver health.
- Curcumin: A compound in turmeric, curcumin supports the liver by reducing fat production in the liver, boosting fat breakdown, and improving insulin sensitivity. Curcumin also has antioxidant and anti-inflammatory effects.
In terms of liver infection, hepatitis C can now be cured in as little as eight to 12 weeks with modern antiviral medicines that are safe and highly effective. Hepatitis B can’t yet be cured, but there are good medications that lower the amount of virus in the body and reduce the risk of long-term damage.
“Prevention isn’t a single action,“ Olsen said. ”It’s a combination of choices that protect your liver every day.”