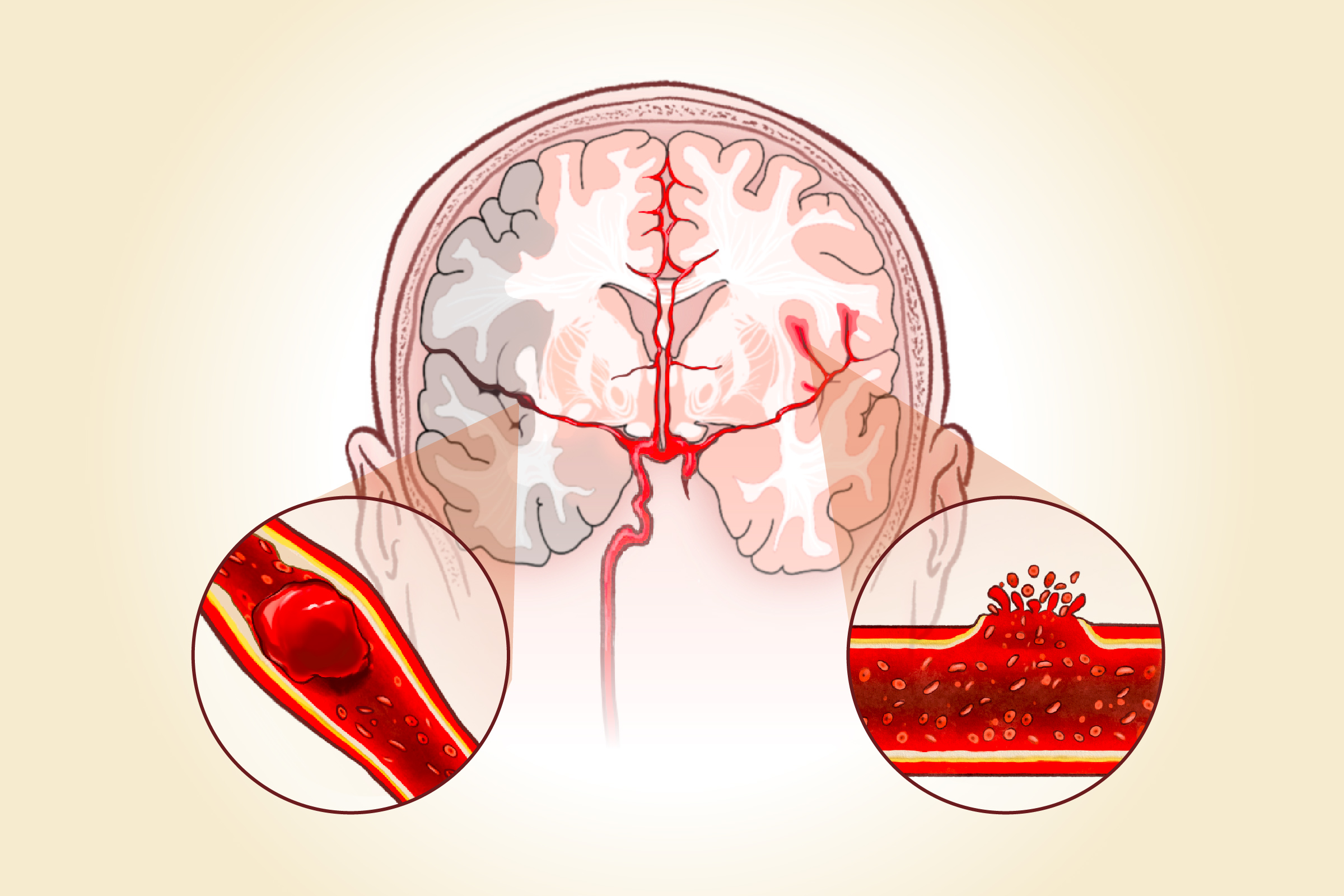
1. Ischemic Strokes
Ischemic strokes, which account for about 87 percent of all strokes, occur when blood flow and oxygen to brain cells are blocked. This blockage usually results from a blood clot or a buildup of plaque in the arteries.
2. Hemorrhagic Strokes
A hemorrhagic stroke occurs when a blood vessel in or on the brain bursts, causing bleeding that leads to brain swelling and increased pressure, which can damage brain cells.
- Substance use: Smoking is a leading preventable risk factor for stroke, as it damages the heart and blood vessels. Secondhand smoke has the same effect.
Excess alcohol intake raises blood pressure and triglyceride levels, which can harden arteries. Alcohol-related stroke risk is high with seven or more beverages per week.
Certain drugs such as amphetamines, cocaine, and cannabis can also raise the risk. Intravenous drug use greatly increases risk due to blood clots that can travel to the brain. - Lifestyle habits: Lack of physical activity increases stroke risk by contributing to obesity, high blood pressure, high cholesterol, and diabetes.
Diets high in trans fats and excess calories carry similar risks. People who drink carbonated beverages regularly also have a significantly higher risk of stroke.
Too little or too much sleep can also increase risk by contributing to high blood pressure, inflammation, and underlying issues such as heart disease or diabetes. - Medical conditions: Heart and blood disorders such as atrial fibrillation and sickle cell disease can increase the risk of blood clots that lead to ischemic strokes. Aneurysms (weakened, bulging arteries), arteriovenous malformations (abnormal tangles of blood vessels), and high blood pressure raise the risk of hemorrhagic strokes. Dyslipidemia—abnormal levels of cholesterol or other fats in the blood—contributes to plaque buildup in the arteries, which increases ischemic stroke risk.
Sleep disorders such as obstructive sleep apnea also increase risk. - Mental health and stress: Anxiety, depression, chronic stress, long work hours, and social isolation can increase stroke risk by raising blood pressure, promoting inflammation, disrupting sleep, and encouraging unhealthy habits.
- Hormone therapies: Oral contraceptives and hormone replacement therapy can raise stroke risk; estrogen especially affects blood-clotting proteins.
- Medications: Anticoagulants, antiplatelet medications, nonsteroidal anti-inflammatory drugs, and some antidepressants may increase bleeding risk by affecting platelets or raise blood pressure.
- Air pollution: Short- or long-term exposure to air particles increases the risk of ischemic stroke by triggering inflammation, oxidative stress, and blood vessel dysfunction.
- Microplastics: Microplastics—tiny plastic particles—carry toxins and have been found in most carotid artery plaques. A 2024 study linked their presence to a 4.5 times higher risk of stroke.
- Transient ischemic attack (TIA): A TIA, sometimes called a mini-stroke, happens when blood flow to part of the brain is briefly interrupted.
- COVID-19 infection: A 2020 study found a strong link between COVID-19 infection and ischemic strokes. Although COVID-19 mRNA vaccines are not established risk factors, a 2024 study found a possible connection, especially in people ages 45 and older, with strokes being reported about eight times more often than expected after vaccination.
Noncontrollable risk factors:
- Gender and age: Men are more likely than women to experience a stroke, but women face a higher likelihood of death when a stroke occurs. Women also encounter elevated risk during pregnancy and menopause due to hormonal changes that affect blood vessels and clotting.
Age is another powerful factor—stroke risk more than doubles with each decade after age 55, although strokes can occur at any age. Even infants under 1 also face higher stroke risk, showing that this medical emergency spans all life stages. - Genetics and family history: Inherited conditions such as blood-clotting disorders like Factor V Leiden or vascular disorders like CADASIL can increase stroke risk and may run in families.
- Race and ethnicity: African Americans have nearly twice the risk of a first stroke compared with Caucasians. Hispanic Americans and American Indian/Alaska Native populations also face higher stroke risk, and both African Americans and Hispanics are more likely to die from stroke.
- Blood type AB: People with type AB blood have about a 24 percent higher risk of ischemic stroke compared with those with type O, according to a large 2023 meta-analysis.
When a person has multiple risk factors, their combined effect amplifies overall stroke risk—making the chance of having a stroke much higher than simply adding each factor individually.
The F.A.S.T. Method
One of the easiest ways to remember stroke warning signs is the acronym F.A.S.T.:
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call 9-1-1
Common Warning Signs
Beyond F.A.S.T., people may experience other sudden symptoms that suggest a possible stroke. The following is a more comprehensive list:
- Numbness, weakness, or paralysis on one side of the body
- Confusion or reduced alertness
- Difficulty speaking or slurred speech
- Vision problems in one or both eyes
- Trouble walking or feeling unsteady
- Dizziness, vertigo, or loss of balance
- Trouble swallowing
- Memory loss
The following symptoms are more common in women
- Pain in the face, arm, or leg
- Hiccups or nausea
- Chest pain or irregular heartbeat
- Difficulty breathing or shortness of breath
When bleeding occurs in the brain—a hemorrhagic stroke, additional symptoms may appear, including:
- Loss of consciousness
- Seizures
- Light sensitivity
- Neck stiffness or pain
- Severe headache with no known cause
- Hand tremors
Imaging Tests
Imaging tests are critical for confirming stroke type, guiding treatment, and ruling out other conditions.
- CT scan: Rules out brain bleeding and shows large damaged areas after about three hours
- MRI with diffusion-weighted imaging: Detects ischemic strokes earlier than CT scans
- Catheter-based angiography: Shows the extent of blood vessel blockages
- Doppler ultrasound: Measures blood flow speed in large vessels and shows whether plaque has narrowed or blocked the carotid arteries
- Echocardiogram: Uses sound waves to find heart clots
Additional Tests
Doctors may also use other tests to identify underlying causes and complications.
- Blood tests: Check blood cells, sugar levels, clotting time, and organ function
- Heart monitoring: Holter monitors track irregular rhythms over several days
- Lumbar puncture: Detects small brain bleeds not visible on CT scans
Artificial intelligence is also being used to support stroke diagnosis. Brainomix 360 Stroke analyzes CT scans in real time, helping doctors make quicker treatment decisions. Studies show it can triple the number of stroke patients achieving functional independence—from 16 percent to 48 percent.
1. Emergency Medicines
Medications are often the first step in stroke treatment, and the approach depends on the type of stroke.
- Tissue plasminogen activator (tPA): The primary treatment, tPA dissolves the blood clot blocking blood flow to the brain and greatly increases the chances of full recovery. It is given through a vein in the arm and is most effective within three hours of symptom onset.
- Blood thinners: Medications such as aspirin or clopidogrel may be given to prevent clots from growing or new ones from forming.
- Neuroprotective drugs: Help shield the brain from damage caused by oxygen loss.
- Osmotic diuretics: Medications such as mannitol may reduce swelling and brain pressure in severe cases.
For hemorrhagic stroke:
- Blood pressure drugs: Lower pressure on blood vessels in the brain.
- Vitamin K: Helps control bleeding.
- Supportive medicines: Manage brain swelling, blood sugar, fever, and seizures.
2. Surgical and Procedural Treatments
Surgical approaches vary depending on whether the stroke is ischemic or hemorrhagic.
- Thrombectomy: Removes clots using a catheter inserted through the thigh.
- Carotid endarterectomy: Removes plaque from the carotid artery in the neck if carotid artery disease caused the stroke.
- Craniotomy: Relieves pressure, removes clots, or repairs bleeding in the brain.
For hemorrhagic stroke:
- Aneurysm clipping: Places a clamp at the base of an aneurysm to block blood flow and prevent rupture.
- Blood transfusion: Replaces lost blood during surgery or injury through a safe intravenous procedure.
- Coil embolization: Inserts a tiny coil into an aneurysm to block blood flow and prevent bursting.
- Drainage: Removes excess brain fluid that builds up and increases pressure.
- Arteriovenous malformation treatment: Uses surgery or radiation to remove or shrink tangled arteries and veins.
- Blood removal: Removes pooled blood if it causes worsening symptoms.
- Craniotomy: May also be used in hemorrhagic strokes to relieve pressure.
3. Rehabilitation
Rehabilitation helps patients recover function and adapt after a stroke.
- Physical therapy: Rebuilds basic movement skills and prevents complications such as muscle tightening or bedsores.
- Occupational therapy: Helps with everyday tasks such as eating, dressing, and bathing.
- Speech therapy: Improves speaking and language comprehension.
- Vocational therapy: Prepares patients to return to work.
- Psychological therapy: Helps manage depression, anxiety, and other emotional challenges.
Newer rehabilitation technologies include:
4. Acupuncture
Acupuncture has long been used in Asia for stroke recovery and is supported by growing research. It may promote brain cell growth, improve blood flow, prevent nerve cell death, balance brain chemicals, and enhance memory and learning. A 2022 study found that acupuncture for ischemic stroke can lower the risk of complications and death. A 2019 study showed that acupuncture helps improve communication in people with post-stroke language disorders. Many clinical studies suggest it may improve overall neurological function.
5. Herbal Medicines
Some herbs may support recovery. They may interact with prescription drugs, so always consult a health care provider before use.
- Ginseng: Reduces inflammation and oxidative stress, but should be avoided by people on blood thinners.
- Astragalus: May help protect the blood-brain barrier.
- Ashwagandha: Reduces inflammation and supports memory improvement.
- Gotu kola: Improves memory and cognitive function.
- Ginkgo biloba: May improve brain function, but should be avoided by people on blood thinners.
- Rosemary: Has antioxidant effects and may help reduce brain swelling.
1. Healthy Habit Changes
Managing medical conditions and adopting healthy lifestyle habits are essential for recovery and prevention.
- Manage atrial fibrillation, diabetes, high blood pressure, and high cholesterol.
- Avoid smoking.
- Limit alcohol to no more than two drinks per week or as directed by a doctor.
2. Brain Exercises
Cognitive activities may help stimulate brain function, improve memory, and support neuroplasticity. Examples include:
- Word puzzles
- Brain teasers
- Board games
- Memory games
- Arts and crafts
- Strategy games
3. Exercise
Exercise improves cardiovascular health, mobility, and independence after stroke. Programs typically include aerobic activity, strength training, and flexibility or balance exercises. Examples include:
- Walking
- Cycling
- Leg raises
- Grip strengthening
- Range-of-motion stretches
The general goal is 150 minutes of moderate aerobic activity per week, tailored to one’s fitness level and post-stroke limitations.
4. Mind-Body Practices
Mind-body practices can help restore physical function and support emotional well-being.
- Tai chi: A 2022 study found that sitting tai chi offers stroke survivors similar or greater recovery benefits compared with standard rehabilitation, with improvements in arm strength, balance, mood, and daily functioning.
- Yoga: Used alongside occupational therapy, yoga supports stroke recovery by encouraging client-centered care and improving both physical and emotional well-being.
- Meditation: Daily meditation can gradually change brain structure in areas linked to attention, emotion, and mental flexibility, promoting calm and focus over time.
5. Diet
A balanced diet helps protect the brain and reduce stroke risk.
- Fish: Any fish consumption reduces stroke risk by about 12 percent, with an additional 2 percent drop per extra weekly serving. Baked or broiled fish, such as tuna, cut ischemic stroke risk by at least 28 percent, while fried fish more than once a week raised risk by 44 percent.
- Soy products: A 2009 study in Chinese women found that those who ate the most soy—such as dried soybeans, tofu, and soymilk—had a 77 percent lower risk of ischemic stroke compared with those who ate the least.
- Vegetables, fruits, and whole grains: A 2014 meta-analysis of 20 studies found that high fruit and vegetable intake lowered total stroke risk by 21 percent, with vegetables offering a greater benefit (23 percent reduction) than fruits (14 percent). Eating three or more servings of whole grains daily can reduce cholesterol and lower the risk of stroke and heart disease.
6. Nutritional Supplements
Supplements may support stroke recovery by improving motor function, cognition, and overall health.
- Vitamin B: Supports brain function; some B vitamins may lower levels of homocysteine, an amino acid linked to higher stroke risk.
- Vitamin D: Supports neuromuscular and bone health. In one small randomized controlled trial, vitamin D and calcium supplementation improved survival rates and functional outcomes in ischemic stroke patients with vitamin D deficiency or insufficiency.
- Vitamins C and E: Enhance antioxidant capacity in patients with acute ischemic stroke.
7. Mental Health Management
Emotional and mental health care is a vital part of recovery. Stroke survivors may experience anxiety, depression, or even post-traumatic stress disorder or psychosis. Helpful measures include:
- Joining a stroke support group
- Using antidepressants or other treatments when appropriate
- Asking family and friends for support
8. Massage
Therapeutic massage may aid recovery when combined with conventional treatment. A 2021 meta-analysis found that Tuina, a traditional Chinese therapeutic massage that stimulates acupoints, improved motor function and reduced spasticity in stroke survivors.
- Avoid controllable risk factors: Reduce exposure to smoking, excessive alcohol, poor diet, physical inactivity, and unmanaged medical conditions.
- Manage chronic conditions: Take medications and adopt lifestyle changes to manage conditions such as high blood pressure, diabetes, and atrial fibrillation.
- Adopt a heart-healthy diet: Eat a high-fiber diet with plenty of fruits and vegetables daily to help lower cholesterol and improve heart health. The Mediterranean diet can reduce ischemic stroke risk by 22 percent, while the Dietary Approaches to Stop Hypertension or DASH diet—recommended by the American Heart Association and American Stroke Association—emphasizes fruits, vegetables, whole grains, and low-sodium foods to support blood pressure control.
- Manage stress: Practice stress-reduction techniques such as exercise, meditation, or counseling.
- Floss daily: A study published in January linked flossing to a 22 percent lower risk of ischemic stroke and a 44 percent lower risk of stroke caused by blood clots from the heart.
Physical Complications
Physical effects of stroke may develop shortly after the event or progress over time.
- Hemiplegic shoulder pain: Affects 24 percent to 64 percent of stroke patients, typically developing two to three months post-stroke
- Blood clots: Limited mobility increases the risk of dangerous clots in leg veins
- Muscle weakness and spasticity: Impairs walking, balance, and daily activities, often leading to falls
- Swallowing difficulties: May cause pneumonia if food or liquid enters the lungs
- Urinary tract infections: Can develop within one to two weeks after stroke and may persist long term
Neurological Complications
Brain-related complications can affect memory, movement, and sensory processing.
- Seizures: Occur in 5 percent to 9 percent of survivors, more common after hemorrhagic strokes
- Cognitive changes: Impair memory, decision-making, and language
- Central post-stroke pain syndrome: Causes chronic nerve pain from brain damage
- Unilateral spatial neglect: Leads to ignoring one side of the body despite intact senses
Long-Term Health Issues
Stroke survivors often face health challenges that continue for years.
- Bone loss: Often affects one side of the body; staying active helps prevent osteoporosis
- Bladder and bowel control problems: May require ongoing management and increase infection risk
- Dementia risk: Survivors face a higher chance of developing dementia
Emotional and Social Complications
Stroke can deeply affect emotional well-being and social connectedness.
- Depression: Affects up to 70 percent of patients with mood changes; 25 percent to 30 percent experience major depression
- Social isolation: Communication difficulties and physical limitations may cause withdrawal from others
- Loss of independence: May create a lasting need for assistance with daily activities