- Lying awake for long periods before falling asleep (more common in younger adults)
- Sleeping only in short bursts or being awake most of the night (more common in older adults)
- Waking up too early and being unable to fall back asleep
- Waking multiple times during the night
Consequences:
- Feeling unrested upon waking or as if one hasn’t slept at all
- Fatigue, low energy, or daytime drowsiness
- Difficulty concentrating
- Irritability, tension, anxiety, or mood swings
- Depression or feelings of frustration about lack of sleep
- Physical symptoms such as headaches, stomachaches, or general aches and pains
- Trouble napping during the day despite feeling tired
1. Acute Insomnia
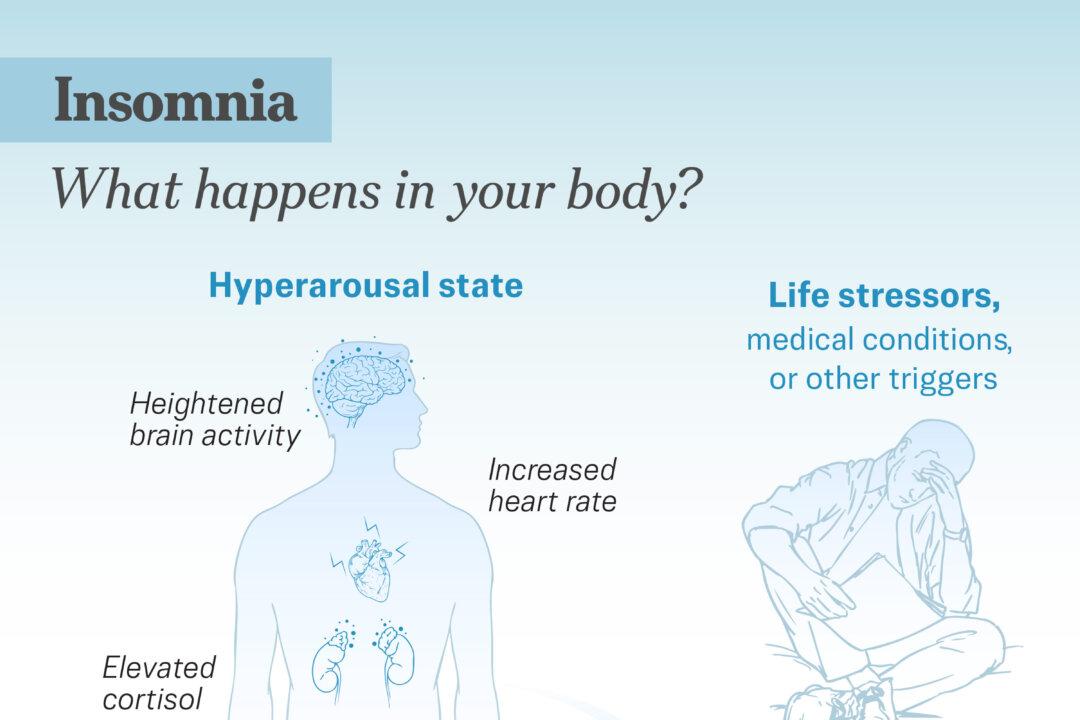
In this case, a sudden trigger pushes your body into a short-term state of hyperarousal. It is temporary, lasting under three months. It can occur in both children and adults, is more common in women, and may appear during pregnancy or menopause. Acute insomnia’s typical triggers include major life events and everyday stresses.
- Stress: Work, school, relationships, or trauma can trigger hyperarousal, making it difficult to sleep and creating a cycle in which insomnia itself adds more stress.
- Lack of Exercise: Reduced daytime activity, especially among older people, can lower sleep pressure. This reduction may lead to more daytime napping and make it harder to sleep at night.
- Certain Substances: Caffeine and nicotine stimulate the body and make falling asleep harder, while alcohol may initially cause drowsiness but ultimately leads to poor-quality sleep.
Having unhealthy sleeping habits may also cause insomnia:
- Mentally Stimulating Activities at Night: Late-night activities such as working, gaming, or using electronic devices can heighten alertness and delay sleep.
- Bed Misuse: Using the bed for activities other than sleep may cause the brain to associate the space with being awake.
- Heavy Meals: Spicy or heavy foods late at night can upset digestion and interfere with sleep.
- Poor Sleep Arrangement: A sleep environment that feels uncomfortable, unsafe, noisy, or too bright can make it harder to fall asleep.
Other triggers involve disruptions to the body’s internal clock:
- Irregular Schedules: Fluctuating bedtimes or inconsistent routines can confuse the circadian rhythm.
- Jet Lag: Travel across different time zones can temporarily shift the body’s internal clock, making sleep more difficult until the rhythm adjusts.
- Shift Work: Sleeping at biologically inconvenient times can disrupt the natural sleep-wake cycle.
- Unhealthy Napping: Late-afternoon naps can disrupt the body’s clock.
Other factors include:
- Injuries or Recent Surgical Procedures: Any condition that causes pain, including injury-induced pain and post-surgical pain, can disrupt sleep. Focusing on the pain while awake also increases stress and makes falling asleep more difficult.
- Female Hormonal Fluctuations: Shifts in hormone levels throughout life can interfere with sleep.
- Pregnancy: Progesterone fluctuations in the first and last trimesters can disrupt sleep.
- Menopause: Intense hormonal changes during perimenopause, along with hot flashes and night sweats, can lead to frequent awakenings.
- Withdrawal of Certain Medicines: Stopping certain drugs can lead to sleep problems due to withdrawal or the body’s adjustment.
Short-term insomnia usually improves once the stressful situation passes or the person adapts or changes his or her habits.
2. Chronic Insomnia
This is a long-standing sleep problem defined as difficulty falling or staying asleep at least three nights a week for three months or more. It may persist continuously or recur in extended episodes.
Other Risk Factors
Beyond medical and psychological causes, several other factors can increase the likelihood of developing insomnia.
- Age: Insomnia is more common in older adults.
- Gender: Insomnia is more prevalent in women than men, partly due to the hormonal changes, as well as higher rates of anxiety and depression.
- Race: African Americans, on average, tend to experience longer sleep onset, poorer sleep quality, and more sleep-related breathing issues compared with Caucasian people.
Medical Evaluation
Your doctor will review your sleep patterns, including bedtime, wake-up time, sleep latency, sleep quality, and actual time spent asleep. They may also ask about daytime habits, lifestyle factors, and your sleep environment, such as caffeine use, exercise, napping, bedroom activities, and household disruptions.
Sleep Diary
Keeping a sleep diary for about two weeks can help diagnose insomnia. Record bedtime, time to fall asleep, number of night awakenings, wake-up time, caffeine or alcohol intake, and any observations from a bed partner. This daily log provides valuable insights into sleep patterns and habits.
Diagnostic Tests
A thorough evaluation may include an exam to check for any medical issues that could be contributing to sleep problems. Several diagnostic tests may be used:
- Sleep Study: In a sleep study, you spend a night in a sleep lab, and your sleep patterns are closely monitored. This can help identify sleep disorders such as sleep apnea, which are not always obvious from a routine examination.
- Actigraphy: This test involves wearing a small wrist motion sensor for three to 14 days to monitor your rest and activity cycles and assess sleep quality.
Discussions about insomnia should encompass your mental and physical health. Addressing both helps your provider develop a comprehensive approach to improving your sleep.
1. Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is usually the first-line treatment for chronic insomnia. It is a 6- to 8-week program designed to help you fall asleep faster and stay asleep longer. Research shows that 70 percent to 80 percent of people with insomnia experience significant improvement after four to six sessions of CBT-I, with benefits often lasting for months or even years. CBT-I includes:
- Cognitive Therapy: Reduces anxiety about not being able to sleep.
- Relaxation Therapy: Uses relaxation techniques to help you fall asleep more easily.
- Sleep Education: Promotes healthy sleep habits.
- Sleep Restriction Therapy: Limits time in bed to improve sleep efficiency and gradually increases it as sleep improves.
- Stimulus Control Therapy: Strengthens the association between bed and sleep by encouraging you to go to bed only when sleepy, leave the bed if unable to sleep, and use the bed only for sleep.
2. Medications
The prescription medications for treating insomnia include:
- Benzodiazepine Receptor Agonists: These medicines help with sleep but may cause anxiety, dizziness, confusion, or muscle weakness. Rarely, they can trigger severe allergic reactions or activities while asleep, such as walking, eating, or driving. They can be habit-forming and are usually prescribed for short-term use.
- Melatonin Receptor Agonists: These medicines can improve sleep but may cause dizziness and fatigue. Rarely, they may cause sleep-related activities or severe allergic reactions.
- Orexin Receptor Antagonists: These medicines are effective for insomnia but not recommended for people with narcolepsy. Rare side effects include sleep-related activities or temporary inability to move or speak when falling asleep or waking.
- Benzodiazepines: These medicines are prescribed only if other treatments fail. They carry risks of dizziness, confusion, muscle weakness, dangerous drug interactions, and dependence, so use is typically limited to a few weeks.
Sometimes, doctors prescribe medications not specifically approved by the Food and Drug Administration (FDA) for insomnia, such as certain antidepressants, antipsychotics, or anticonvulsants, to help improve sleep.
3. Over-the-Counter Sleep Aids
They include over-the-counter medications and dietary supplements. However, it is important to pay close attention to potential risks and side effects.
- Melatonin Supplement: Melatonin is a natural hormone released by the brain about four hours before sleep, triggered by reduced light exposure at night. Melatonin supplements are available over the counter in pill form. Since these supplements are unregulated by the FDA, dosages and ingredients can vary between brands, so it’s recommended to stick with a single trusted brand and avoid unknown sources. However, long-term use of melatonin supplements for sleep may pose potential health risks, such as heart failure. It’s better to adopt a healthy lifestyle or use other approaches that target the root cause.
- 5‑Hydroxytryptophan (5‑HTP) Supplement: Disruptions in the gut microbiome can interfere with the production of neurotransmitters and hormones—particularly serotonin and melatonin—which are essential for regulating the sleep-wake cycle. A 2024 study found that 5-HTP supplementation can enhance certain aspects of sleep quality in older adults, especially in those with poor sleep, and may also improve gut microbiota composition.
- Sleep Medications With Antihistamines: Diphenhydramine and doxylamine succinate are sedating antihistamines found in many over-the-counter sleep and allergy medications. They promote sleep by reducing histamine levels in the brain and helping the body feel ready for rest.
4. Light Therapy
Light therapy uses light exposure to adjust your circadian rhythm, especially if you tend to sleep and wake earlier than desired. Treatment may involve using a lightbox or spending time outdoors in the evening.
5. Vagus Nerve Stimulation
Vagus nerve stimulation activates the parasympathetic “rest and digest” response and reduces sympathetic overactivity, influencing brain regions that regulate stress and the sleep-wake cycle. it can also modulate key sleep-related neurotransmitters such as GABA and serotonin and enhance deep sleep brain waves. Vagus nerve stimulation can be performed either mechanically with devices or naturally. Nondevice methods such as diaphragmatic (belly) breathing offer similar benefits; by slowing the breath and lowering stress hormones, this technique triggers relaxation and improves sleep. A 2021 study showed that four weeks of diaphragmatic breathing can increase sleep duration, reduce disturbances, and enhance overall sleep quality and daytime functioning.
6. Acupuncture
Acupuncture may be particularly beneficial for people whose insomnia is related to depression, menopause, or chronic pain. Regular treatments over one to two months can improve sleep quality, reduce nighttime awakenings, increase total sleep time, decrease anxiety, and alleviate pain.
7. Herbs
Some herbs may help promote relaxation and improve sleep when used safely and appropriately.
- Chamomile: Chamomile is a gentle natural sedative that can help relax the nervous system and promote sleep. Its flowers contain bioactive compounds that contribute to its calming effects. Apigenin, in particular, is thought to be the main compound responsible for chamomile’s sleep-promoting and anxiety-reducing properties. A 2024 study found that chamomile enhanced sleep quality by reducing nighttime awakenings and helping with sleep maintenance, but it did not increase overall sleep duration.
- Valerian Root: A traditional herbal remedy, commonly taken as a tea, capsule, or tablet, valerian root may promote relaxation and improve sleep by affecting gamma-aminobutyric acid or GABA—one of the most important inhibitory neurotransmitters in the brain—and serotonin receptors. Although its exact mechanism is unclear. Valerian is generally safe for short-term use. It should not be combined with sedatives, alcohol, or certain medications, and is not advised for young children, pregnant women, or women who are breastfeeding.
- Jujube Seed Herbal Tea: Jujube seeds promote relaxation, reduce anxiety, and support heart health, while Poria cocos extract helps people fall asleep faster and sleep longer. You can make a calming sleep-support tea by simmering the herbs in water and drinking it every afternoon. Mild sleep issues may improve after one to two weeks, while chronic problems may require longer, consistent use.
- Kava: A plant native to the Pacific Islands that has been used for centuries to help with relaxation and sleep. Its root contains natural compounds called kavalactones, which may help calm the brain by affecting chemicals such as GABA, serotonin, and dopamine. Research shows that kava can reduce anxiety and may improve sleep, especially when stress or anxiety interferes with rest.
- Passionflower: Known for its calming effects, it can help reduce anxiety and support restful sleep.
8. Hypnotherapy
A 2018 systematic review of 24 studies suggests that hypnosis may be a promising treatment for sleep problems, with over half of the studies reporting benefits for sleep outcomes. It appears to be generally safe, with a low incidence of adverse effects, although further investigation is needed to confirm its effectiveness.
1. Essential Oils
Essential oils, extracted from aromatic plants, are used in aromatherapy to support mental health and well-being. Research shows that essential oils such as lavender and bergamot can improve sleep quality and duration, and reduce sleep deprivation in both healthy people and those with sleep problems. They are generally considered a safe complementary therapy.
2. Sleep-Improving Foods
Certain foods can naturally support better sleep by providing nutrients and compounds that promote relaxation and regulate the sleep-wake cycle.
- Melatonin-Rich Foods: Tart cherries (including Montmorency cherries), unsweetened tart cherry juice, pistachios, almonds, eggs, and milk can help signal the body that it’s time to sleep.
- Tryptophan-Containing Foods: This amino acid converts into serotonin and melatonin in the body and may improve sleep quality. Examples include turkey, chicken, fish, eggs, cheese, edamame, tofu, peanuts, quinoa, banana, and pumpkin seeds.
- Magnesium-Rich Foods: These foods can support relaxation and help regulate sleep. Spinach, avocados, bananas, and sweet potatoes are good sources of magnesium that may contribute to a more restful night’s sleep.
- Tart Cherry: Tart cherries are rich in sleep-promoting compounds, including melatonin, tryptophan, serotonin, and proanthocyanidins.
3. Meditation
Meditation is a type of mind-body therapy that combines mental focus with physical practices such as deep breathing. Sleep meditation reduces anxious thoughts and physical stress, promoting overall relaxation. By triggering the body’s relaxation response—slowing heart rate, lowering blood pressure, and calming brain activity—it counteracts the stress response and creates conditions more conducive to sleep.
4. Music Therapy
Music therapy is widely used to improve sleep in people with insomnia. It works primarily by inducing physiological relaxation, reducing arousal, and regulating mood and anxiety. It may also increase beta-endorphins (natural chemicals that promote relaxation), modulate serotonin (a neurotransmitter that influences the sleep-wake cycle), and decrease sympathetic activity. A review published in January involving 27 studies confirmed its effectiveness in enhancing subjective sleep quality.
5. Spa Therapy
According to a 2023 systematic review, hydrotherapy (the therapeutic use of water), balneotherapy (bathing in mineral-rich waters), and other spa treatments may improve sleep quality and duration by influencing key hormones such as histamine and serotonin, calming the nervous system, and helping regulate body temperature. The review also found that hot spring bathing can improve sleep by adjusting core body temperature. Hot spring spa therapy appears especially effective for people with difficulty falling asleep, as it reduces pre-sleep rumination and shortens the time it takes to fall asleep.
6. Exercising
Regular exercise improves sleep quality through several mechanisms: it reduces stress, enhances mood, regulates body temperature, and can boost melatonin production. Post-exercise cooling promotes sleepiness and facilitates sleep onset. However, evening exercise may sometimes delay or suppress melatonin release, potentially affecting sleep initiation and quality. A meta-analysis published in July found that different types of exercises, such as yoga, tai chi, and walking or jogging, were more effective in improving sleep than other forms of physical activity.
7. Aerobic Dancing
A 2023 study involving community-dwelling adults over 60 with both mild cognitive impairment and poor sleep found that a 16-week aerobic dancing program improved sleep quality and cognitive function.
- Create a bedroom environment that is cool, quiet, and dark.
- Ensure your sleep surface is comfortable, with a mattress and pillows that provide proper support.
- Use tools such as blackout curtains, eye masks, fans, or sound machines to enhance comfort.
- Go to bed only when you feel sleepy; if you cannot fall asleep, get up and do a quiet activity in another room until sleepiness returns.
- Maintain healthy daytime habits to support nighttime sleep.
- Get regular physical activity—ideally at least five to six hours before bedtime—and eat meals on a consistent schedule while avoiding late-night dinners.
- Limit fluids close to bedtime to reduce nighttime bathroom trips.
Don’ts:
- Avoid TV or electronic devices before bed, as their light can disrupt your sleep-wake cycle. Modern exposure to artificial light from phones, computers, and TVs can suppress melatonin production, making it harder to fall asleep.
- Avoid stimulating activities and stressful situations before bedtime, such as checking social media, having intense discussions, or catching up on work.
- Reserve your bedroom for sleep only, and avoid reading, worrying, or watching television in bed.
- Limit daytime naps. If a nap is necessary, keep it under 30 minutes and finish before 3 p.m.
- Limit intake of caffeine, nicotine, and alcohol in the evening. While alcohol may help you fall asleep initially, it can disrupt sleep later in the night, leading to lighter, fragmented sleep.
- Be aware that certain over-the-counter or prescription medications, including some cold or allergy medicines, can interfere with sleep.
- Inflammation: Elevated systemic inflammation, measured by circulating C-reactive protein levels, is independently linked to a higher risk of cardiovascular disease and mortality.
- Heart Disease: Chronic insomnia is associated with a higher likelihood and greater severity of long-term cardiovascular conditions, including high blood pressure and heart disease.
- Hypertension: Chronic sleep deprivation increases stress hormone levels, raising blood pressure over time.
- Obesity: Lack of sleep disrupts appetite-regulating hormones, leading to increased hunger and weight gain.
- Diabetes: Sleep loss impairs insulin sensitivity, making it harder to regulate blood sugar.
- Stroke: Poor sleep contributes to cardiovascular strain and inflammation, increasing stroke risk.
- Tension Headaches: Sleep disruption elevates stress and muscle tension, triggering headache pain.
- Mental Health Conditions: Examples include depression and anxiety.
- Injury: Increased risk of injury, including being involved in a car accident due to drowsy driving.








