Stressful events such as the death of a parent, a divorce, or a severe illness experienced in childhood or midlife may make us more susceptible to developing Alzheimer’s later, a recent study has found.
The findings appear in a March review article in The Annals of Neurology.
Study Details
Chronic stress affects the function and structure of the brain, and increasing
evidence suggests it also plays a role in the development of Alzheimer’s. The March study examined the associations of accumulated “stressful life events” and their effects on different biomarkers associated with Alzheimer’s—including gray matter volume and brain inflammation.
The study involved 1,290 participants who were at an increased risk of developing Alzheimer’s—because most were descendants of a family member living with the disease. The group was otherwise “cognitively unimpaired” and 45 to 74 years old.
The researchers looked at 18 specific stressful life events and when they occurred in the participant’s lives. The stressful life events the study evaluated were:
- Death of mother
- Death of father
- Separation of parents
- Victim of abuse
- Terminated pregnancy
- Disabled child
- Divorce
- Death of a partner
- Death of a child
- Death of a close one
- Major illness of a close one
- Major illness
- Institutionalization
- Becoming unemployed
- Retirement
- Economic loss
- Legal problems
- Economic problems in childhood
The study defines these events as “likely to bring about readjustment-requiring changes in individuals’ lives.” However, depending on how each person processes the experience, they could also be categorized as traumatic events—but more on that later.
A small portion of the group (393 out of 1,290) had samples of spinal fluid taken to scan for the presence of amyloid and tau proteins—proteins associated with Alzheimer’s disease.
The researchers also assessed the volume of gray matter in the participants’s brains. Gray matter is vital to receiving and processing information from our environment. There is often a reduction in gray matter in people with Alzheimer’s.
The researchers also evaluated inflammation in the brain, which is thought to be one of the central mechanisms of Alzheimer’s disease.
Inflammation in the Brain
Over the past decade, inflammation in the brain has emerged as one of the core pathologies of Alzheimer’s disease, along with the presence of amyloid beta plaques and neurofibrillary tangles, according to
a study published in Alzheimer’s and Dementia in 2018.
Multiple investigations have shown that, in addition to amyloid beta plaques and neurofibrillary tangles, there was evidence of prolonged and sustained inflammation in the brains of patients with Alzheimer’s. This inflammatory response has been observed in Alzheimer’s patients post-mortem and the early stages of the disease, before diagnosis, the study found.
The same study found that chronic inflammation in the brain is not unique to Alzheimer’s, and increased inflammation has been observed in the brains of people with Parkinson’s disease, amyotrophic lateral sclerosis, and multiple sclerosis.
The root of inflammation in the brain is microglia—the brain’s immune cells. These cells are vital to brain health and outnumber our neurons 10 to one. Microglia have the crucial function of clearing out dead neurons and other debris, including beta-amyloid plaques and helping to contain the spread of tau proteins—keeping the brain in optimal working order.
When inflammation occurs in the brain, because microglia are on the offensive, communication between neurons slows down, hindering their energy production. This leads to symptoms ranging from brain fog and sluggish thinking to difficulty concentrating. Long-term inflammation leads to neuronal death and the development of neurodegenerative disorders such as Alzheimer’s and other dementias.
Stress is vital for survival, and increased levels of hormones such as cortisol and adrenaline (which activate our fight-or-flight response) are crucial to avoid dangerous situations. However, when stress is prolonged, the ongoing release of these hormones can lead to inflammation and result in a cascade of serious health consequences.
Study Results
The researchers found that stressful events in childhood and midlife were associated with abnormal amyloid beta and tau proteins in the brain, which are considered biological markers of Alzheimer’s. However, they did not find that stressful events reduced gray matter volume overall.
The study suggests there is a connection between trauma in childhood and inflammation. “Our results are in line with emerging evidence suggesting childhood trauma to be linked with increased adulthood inflammation and evidence suggesting that the risk of developing chronic inflammation is affected by early development and persists throughout the life course to affect health later in life.”
Several studies have also suggested that midlife is when the biological markers of Alzheimer’s begin to accumulate in the brain and research suggests that intensely stressful events may affect or even accelerate that process.
Other findings from the study were that total stressful events were associated with amyloid beta proteins, neuroinflammation, and a reduction in gray matter, but only in people who had a history of psychiatric disorders.
The results also differed between men and women.
For the women in the group, total stressful life events were associated with reduced gray matter, but the same was not true for the men. In the men, total stressful life events were associated with tau proteins, but the same was not true for the women. Although the study didn’t determine why, it could be the difference in how men and women respond to stress—physically as well as psychologically.
Stress, Trauma, and the Brain
The death of a parent, going through a divorce, losing a job, or being diagnosed with an illness are things that many of us will experience, and experts who study trauma are beginning to understand that these adverse events that we all experience can change the brain and alter the way we perceive our world.
A simple definition of trauma is an event that overwhelms our ability to deal with it in the moment. Trauma is the impact of ongoing or intense stress.
In his film The Wisdom of Trauma, Dr. Gabor Mate, a physician, bestselling author, and expert in trauma and addiction describes trauma this way, “Trauma is not the bad things that happen to you, but what happens inside you as a result of what happens to you.” Trauma is how we respond to the things that happen to us and not the events themselves.
An article published in Chronic Stress explains the effects of stress on the brain. “The brain is the central organ of stress and adaptation to stress because it perceives and determines what is threatening ...”

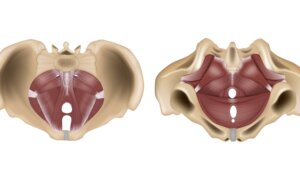
The limbic system (decade3d - anatomy online/Shutterstock)
An article published in Dialogues in Clinical Neuroscience states that trauma affects three parts of the brain: the amygdala, the hippocampus, and the prefrontal cortex.
The amygdala is located deep inside the brain and is part of the limbic system. It’s involved in emotional and behavioral responses, especially those needed for survival. The amygdala is a tiny, almond-shaped structure responsible for processing emotions and controlling our fear response. When the amygdala detects a threat, it activates our fight, flight, or freeze response.
The hippocampus is the part of the brain that processes emotions and is critical to forming and retaining long-term memories. When a threat is detected, the hippocampus signals the release of cortisol, a stress hormone that diverts all the body’s resources to functions it needs to survive the threatening situation. It also shuts down nonvital functions, such as digestion, giving us the best chance at survival.
In a study published in Biological Psychology, brain scans revealed that after trauma, the hippocampus got smaller.
The prefrontal cortex is the part of the brain responsible for higher-level thinking, reasoning, problem-solving, and logic and governs focus and attention.
A study published in Neurobiological Stress explored the stress response, post-traumatic stress disorder, and their effects on the prefrontal cortex. It found that dysfunction in this area of the brain caused by trauma could lead to behavior changes that include “aggressive and irritable behaviors, outbursts of temper, reckless behavior, problems with concentration on tasks requiring vigilance such as schoolwork, and sleep disturbances.”
An article in Stat Pearls discusses the physiology of the stress response, explaining that when these systems work correctly, they react to the perceived threat and then return to normal after the danger has passed, a reaction called acute stress. Chronic stress or trauma, however, which the article breaks into traumatic, environmental, psychological, and physiological, causes a wide range of problems, and undermines health and well-being.
An overly active amygdala causes us to sense danger everywhere (even when there is none). It can lead to anxiety and depression, as well as other negative effects on our health, including inflammation.
A systematic review published in Psychopharmacology examined the effects of psychosocial stressors on microglia (the brain’s immune cells) and their implications for mental illness. The review concluded that “a range of psychosocial stressors lead to elevated microglial activity in the hippocampus and good evidence that this is also the case in other brain regions.”
The continued release of stress hormones such as cortisol and adrenaline can also have negative consequences. For example, prolonged cortisol levels can cause a weakened immune system and make people more prone to illnesses and infections. Studies have shown that heightened levels of cortisol over extended periods can lead to high blood pressure, diabetes, atherosclerosis, and inflammation.
These experiences also seem to have a more profound impact on childhood, and studies show that victims of childhood trauma are much more likely to suffer from chronic diseases as adults.
Neuroplasticity
While the above study points to these adverse events having the potential to change our brains and lead to problems such as neurodegenerative diseases later on, one factor gives us hope that the brain has the potential to heal itself—neuroplasticity.
Neuroplasticity is the brain’s ongoing changes and reorganization in response to its environment. This ability to adapt and change allows the brain to heal from traumatic events. A study published in Biological Psychiatry showed that reduced volume in the hippocampus was reversible when stress and its corresponding cortisol levels were reduced.
Other studies demonstrate that targeting neuroplasticity may be an effective tool in addressing neurodegenerative diseases.
One review published in Translational Neurodegeneration in 2020 used different brain stimulation techniques to target neuroplasticity in patients with Alzheimer’s and Parkinson’s disease. Although still in the research phases, the authors concluded that “targeting the impaired neuroplasticity with improved brain stimulation techniques could offer a powerful novel approach for the treatment of AD [Alzheimer’s disease] and PD [Parkinson’s disease].”
An editorial article published in Frontiers in Neuroscience evaluated the benefits of exercise-induced neuroplasticity. Resistance exercise, in particular, was found to reduce amyloid beta deposition, neuroinflammation, and neurofibrillary tangles in human and animal models of Alzheimer’s disease, and was recommended “as a possible therapeutic strategy, not only to improve symptoms, but also to prevent or control the progression of neurodegeneration in AD.”
Final Thoughts
Although there are no guaranteed ways to avoid Alzheimer’s,
The Alzheimer’s Association offers 10 healthy habits to improve brain health and reduce the risk of cognitive decline and, perhaps, Alzheimer’s and dementia as well.
- Keep your brain engaged
- Be a lifelong learner
- Exercise regularly
- Protect your head—always wear a helmet and seat belt when appropriate to protect your head from injuries
- Don’t smoke
- Control your blood pressure
- Manage diabetes
- Eat a healthy diet
- Maintain a healthy weight
- Get good quality sleep
By making mindful choices, we empower ourselves to maintain optimal brain health now and preserve it well into the future.