Have you ever been out with friends, laughing a bit too hard—when suddenly, a little pee escapes? Or maybe a sneeze catches you off guard with the same embarrassing result? Does the thought of running, lifting weights, or jumping on a trampoline make you break out in a cold sweat? If this sounds all too familiar, you’re not alone—millions are right there with you.
Welcome to your pelvic floor.
The pelvic floor is a group of muscles and ligaments whose strength prevents incontinence of the bladder and bowel, supports the pelvic organs, and is vital to sexual function.
When the pelvic floor functions correctly, so do essential bodily processes, and we hardly give it a second thought. But when issues occur—like bladder or bowel leakage, painful sex, or organ prolapse—the discomfort and embarrassment can be overwhelming. These symptoms are more common than many realize, and people need support and reassurance that they are not alone. So, let’s start the conversation.
The Pelvic Floor
In addition to their role in many vital bodily functions, the pelvic floor
muscles work in concert with other major muscle groups in our core to help our bodies absorb external pressure from lifting, sneezing, coughing, running, jumping, laughing, and so forth, while protecting our spine and other organs.“Our pelvic floor is really one-quarter of what we would consider our core,” Michelle Weeks, a board-certified pelvic floor specialist with a doctorate in physical therapy, told The Epoch Times. “And it’s a muscle group that is pretty much always active, so it never really turns completely off—which is good because we don’t want it to—that’s how we maintain our continence,” she said.
Weeks says the pelvic floor coordinates with other muscles, such as the abdominal muscles, diaphragm (breathing muscle), and deep back muscles.
“The goal of our core is to maintain a consistent amount of pressure for everything that resides within it. So, all of our blood vessels, our organs, things of that nature—they don’t like too much pressure,” she said.
In addition to providing support for internal organs such as the bladder, uterus, and rectum, the pelvic floor helps prevent bladder and rectal leakage caused by pressure inside the abdomen, Kari Bø, a trained physical therapist, professor, and expert in pelvic floor exercise and incontinence research with a PhD in physiotherapy and exercise science, told The Epoch Times via email.
Sex Differences
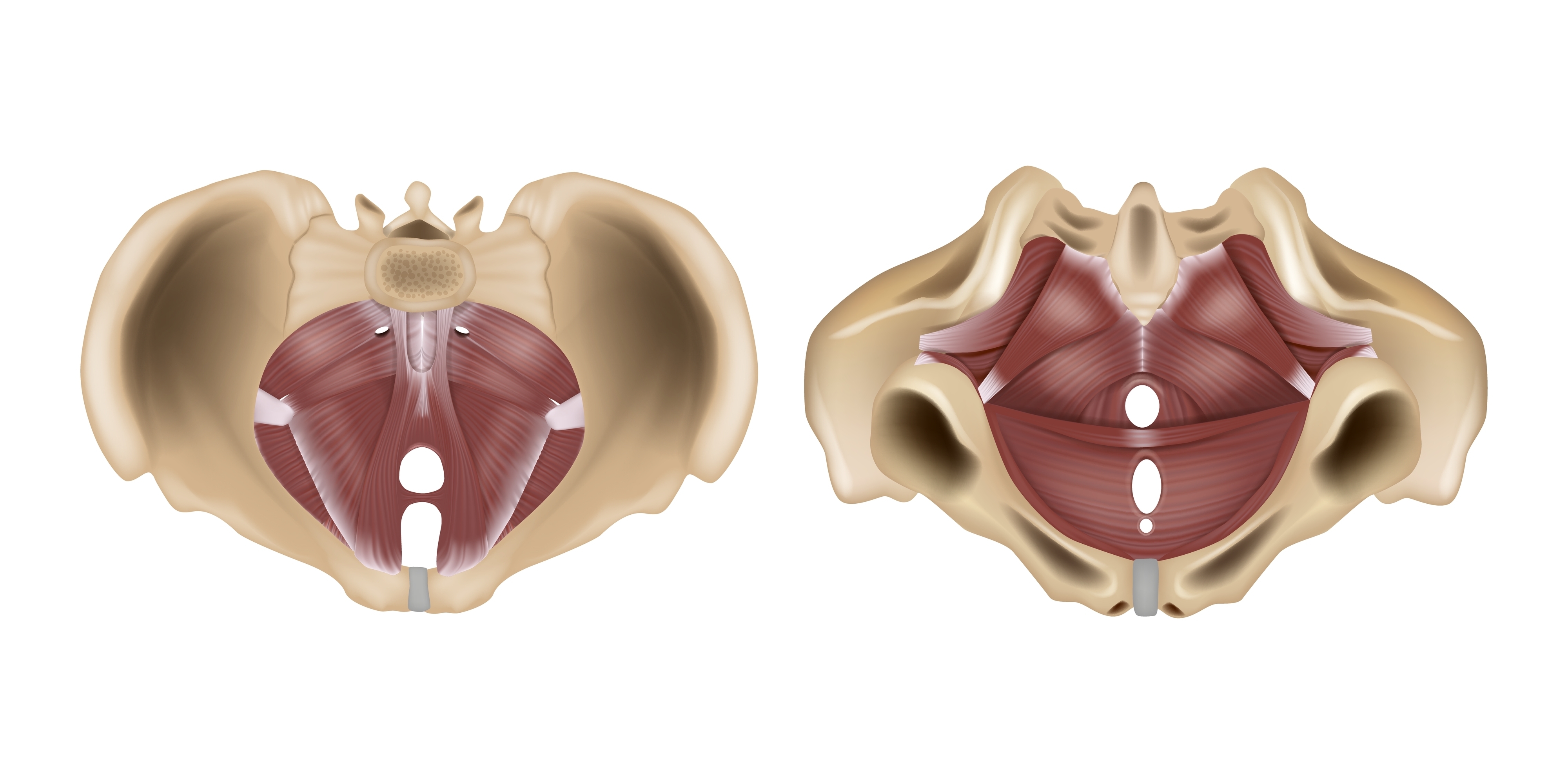
There are differences in the pelvic floor between men and women, too.
Bø says that men’s pelvises are narrower than women’s, and they only have two openings (the urethra and anus) compared to women, who have three (the urethra, anus, and vagina). For women, pregnancy and childbirth dramatically affect the pelvic floor.
Bø says the combination of hormones during pregnancy and the added weight of the baby stretches and opens the pelvic floor. While this is crucial for childbirth, it can lead to problems—damaging the pelvic floor muscles and the perineum (the area between the vagina and anus).
Men have a longer urethra and a prostate to keep urine from leaking, but with age, they have the opposite problem, Bø added.
“As the prostate grows, they may experience problems in urinating/having weak urine stream—while women tend to leak,” she said.

(VectorMine/Shutterstock)
Pelvic Floor Issues
Problems with the pelvic floor can be due to a variety of factors, including pregnancy and childbirth, surgeries like hysterectomy, obesity, chronic constipation, heavy lifting, chronic coughing, and anything that puts additional pressure on these critical muscles and ligaments.
Weeks adds that athletic injuries, car accidents, and trauma—even emotional trauma—can impact the pelvic floor and its function.
“When things go awry is when those muscles either become too weak, or, potentially on the other side of the spectrum too, they become restricted and they’re not able to relax and move through their full range of motion,” Weeks said.
Problems also differ between women and men.
Scope of Pelvic Problems
Urinary incontinence (UI) is widespread, and there are currently an estimated 13 million people directly affected in the United States.
The overall prevalence of urinary incontinence is twice as common in women than in men, and there are five different types—stress urinary incontinence, urge urinary incontinence, mixed urinary incontinence, overflow urinary incontinence, and functional urinary incontinence, according to StatPearls.
Types of Incontinence
One of the most common issues is involuntary urine leakage during various activities. Weeks says it can happen due to coughing, jumping, sneezing, or picking up your kids—and is called stress urinary incontinence, or SUI. SUI occurs because the activity generates too much pressure for the system to handle, causing leaks.
SUI is especially common in women after childbirth (vaginal or via C-Section) and in older people. StatPearls estimates that 24 percent to 45 percent of women over 30 have stress urinary incontinence.
Weeks says that although SUI is more prevalent in women, there are circumstances when it becomes common in men.
“After prostate removal—so, in the instance of prostate cancer—men have a lot of stress incontinence that we’re going to be working on and just making sure that we’re getting those muscles to activate again after they were disrupted from surgery,” she said.
Bø says the other type of urinary incontinence that is common in those with pelvic floor issues is urge urinary incontinence, or UUI, which she describes as involuntary leakage that usually precedes the urge to urinate. The condition can lead to the person not reaching the bathroom in time.
The prevalence of UUI in the United States is:
- 22 percent of women
- 9 percent of women aged 40–44
- 31 percent of women over 75
- 42 percent of men over 75
Risk of Prolapse
Other concerns that can arise from a dysfunctional pelvic floor are pain during sex, constipation, diarrhea, back pain, erectile dysfunction, and pelvic organ prolapse, or POP—which can happen with the uterus, bladder, or bowel.
POP occurs when one or more of the pelvic organs slips out of its normal position and can descend into (or out of) the vagina, or rectum. Prolapses can happen to men and women but are more common in women. Although not life-threatening, they can be painful and highly uncomfortable.
Prevention and Treatment
The good news is that, despite the prevalence of pelvic floor problems, there are ways to treat them—and many can be resolved without surgery.
Weeks says two types of specialists deal specifically with the pelvic floor—pelvic floor physical therapists and pelvic floor occupational therapists.
“There might be some good programs that personal trainers have developed, but they’re not going to have the depth and breadth of education as a PT [physical therapist] or an OT [occupational therapist] that specializes in the pelvic health realm,” she said.
Pelvic Floor Muscle Training
One standard physical therapy treatment for problems with the pelvic floor is pelvic floor muscle training, or PFMT—a group of exercises designed to strengthen the pelvic floor muscles.
PFMT is one of the most commonly used treatments for women with SUI but is also recommended for men with stress urinary incontinence, which is common after prostate surgery, for those with fecal incontinence, and other types of urinary incontinence.
“Pelvic floor muscle training (PFMT) has international consensus to be [a] first-line treatment for UI and POP, meaning that it has shown to be effective in high-quality randomized controlled trials and systematic reviews,” Bø said.
Bø states that if, after three months of intensive, supervised PFMT therapy, there is no improvement, surgery can be an option.
Bladder Training
Another treatment for urinary incontinence is bladder training, Bø continued. According to the Cleveland Clinic, bladder training entails a series of techniques that train the bladder to hold more and empty less often.
Pessaries
Both Weeks and Bø mentioned that a pessary can be a good option for some women with pelvic organ prolapse.
Pessaries are small devices that are placed into the vagina to support the prolapsed organ. They come in many shapes and sizes, and a health care practitioner can help fit a pessary and assist in finding which type is best suited to individual situations.
Some pelvic floor therapists can also fit and order pessaries for patients.
“What we’re seeing now [is] that pelvic floor therapists with additional training are allowed to fit and order pessaries for patients, and that [for] people who utilize them—sometimes after a few years—tissue is actually healed and that prolapse has improved,” Weeks noted.
Improving Pelvic Floor Health
If you struggle with any of the above conditions, improving pelvic floor health can be as simple as making good lifestyle choices.
Weeks says eating well, staying hydrated, managing stress, incorporating movement you enjoy into your life, and having daily healthy bowel movements (which should be easy and not require straining) are critical to pelvic floor health. Another is listening to our bodies.
“Making sure that we are aware of what’s going on in our body, that we’re not ignoring our hunger cues, our thirst cues, that we’re sleeping well, we’re managing our stress—that can go a long way to keeping our pelvic floor healthy,” she said.
Bø adds that avoiding straining or pressing downwards and weight gain can help to protect pelvic floor health.
Final Thoughts
If you are concerned about your pelvic floor health or experiencing symptoms, consult with your physician and seek a qualified physical or occupational therapist to see how they can help. Even if there aren’t any in your area, some practitioners and clinics offer remote appointments to give patients information, support, and guidance.
Weeks says that stress urinary incontinence is extremely common but can often be resolved relatively easily. Unfortunately, many people suffer in silence, believing it’s normal and something they have to live with.
“Unfortunately, pelvic floor dysfunctions are still taboo areas, and both men and women may feel embarrassed about the conditions and are reluctant to seek help,” Bø says.
She says this is unfortunate because improvements and even complete reversal of many problems are possible.
While surgery may sometimes be necessary, there are many other effective treatments for pelvic floor issues. Most importantly, you don’t have to suffer in silence. Pelvic floor problems are common, and help is available. If you’re experiencing difficulties, seek professional care—the help and support you deserve is waiting for you.