Common Early Signs
Lupus often develops gradually, with early symptoms that can be easy to overlook. Recognizing these warning signs may help with earlier diagnosis and management.
- Extreme fatigue: Often the first and most persistent symptom
- Joint pain and swelling: Commonly affects hands, wrists, and knees
- Skin rashes: Including the characteristic butterfly rash across the nose and cheeks
- Fever: Particularly fever exceeding 100 degrees Fahrenheit, linked to inflammation
- Sensitivity to sunlight (photosensitivity): Can trigger rashes, fever, fatigue, or joint pain
- Muscle pain: Often affecting the neck, thighs, shoulders, and upper arms
- Headaches: May be accompanied by memory problems or confusion
Advanced Symptoms by System
As lupus progresses or becomes more active, it can affect nearly every system in the body. Symptoms often extend beyond the early warning signs, affecting major organs, appearance, and even cognitive function. Not everyone with lupus will experience all of these issues, but understanding them can help people recognize when the disease may be flaring or evolving.
- Muscle and joint pain, stiffness, and swelling affecting multiple areas
- Arthritis development in the joints
Skin and appearance changes:
- Mouth sores on the lips or inside the mouth
- Patchy hair loss linked to disease activity, medications, or infections
- Eye inflammation and eyelid rashes
- Discoloration in the fingers and toes
- Various rashes depending on lupus type
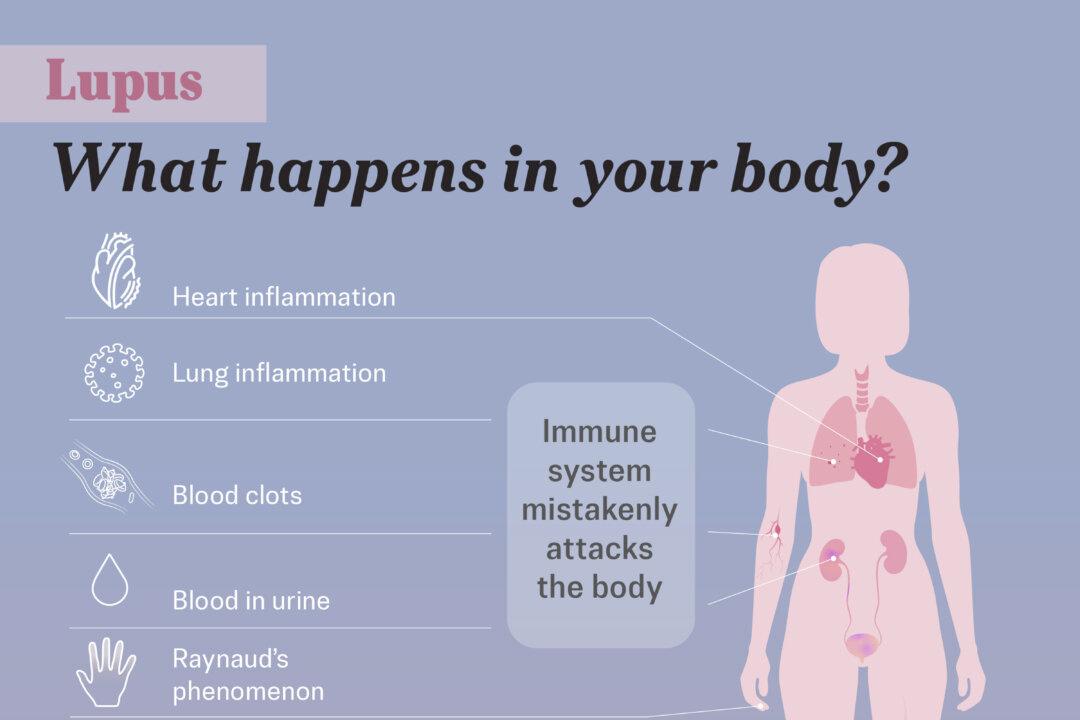
Cardiovascular and blood disorders:
- Chest pain from lung lining inflammation (pleuritis)
- Anemia leading to severe fatigue and weakness
- Elevated blood clot risk that may cause stroke, heart attack, or recurrent miscarriages
- Abnormal blood cell counts, including low white blood cells or platelets
Gastrointestinal issues:
- Abdominal pain
- Heartburn from gastroesophageal reflux disease
- Peptic ulcers caused by lupus medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids
Eye and glandular problems:
- Dry, inflamed eyes
- Sjögren’s syndrome, a condition that damages tear and saliva glands and causes dryness in the eyes, mouth, and vagina
Endocrine and metabolic issues:
- Weight fluctuations due to lupus activity or medications
- Swelling in the legs or around the eyes
Cognitive symptoms:
- Brain fog
- Memory loss
- Difficulty concentrating
Risk Factors of Lupus
While the exact cause of lupus remains unclear, research points to a combination of genetic, environmental, and hormonal factors that can increase a person’s risk. Some of these factors are beyond a person’s control, but others, like certain lifestyle triggers, may be avoidable.
- Family history: A 30 percent concordance in identical twins and 5 percent to 10 percent in fraternal twins
- Gene variations: Multiple variations related to immune system function
- Rare gene mutations: Mutations that can directly cause the condition
Environmental triggers:
- Ultraviolet light exposure: Sunlight can trigger symptoms and flares
- Cigarette smoke: Includes both smoking and secondhand smoke exposure
- Viral infections: Infections such as cytomegalovirus or Epstein-Barr virus
- Severe stress: Life events like divorce, illness, or the loss of a loved one
- Major surgeries or injuries: Physical trauma that may trigger disease activity
- Vitamin D deficiency: Low levels that may affect immune system regulation
- Toxic exposures: Substances such as silica, mercury, or cigarette smoke
Demographic factors:
- Sex: 90 percent of adult cases occur in women, largely due to hormonal influences, particularly estrogen
- Age: Most diagnoses occur between 15 and 44, though 20 percent of SLE cases occur in people over 50
- Race and ethnicity: Higher prevalence in nonwhite populations in the United States
- Geographic location: Increased incidence in industrialized countries, with a 10 percent rise over 50 years in Western nations
1. Systemic Lupus Erythematosus (SLE)
SLE is the most common form of lupus. It can affect multiple organs, including the skin, joints, kidneys, heart, lungs, and brain. SLE is the most widely recognized and commonly diagnosed form of lupus.
2. Cutaneous (Skin) Lupus
Cutaneous lupus occurs when the immune system attacks skin cells, leading to inflammation and rashes that are often red, thick, and scaly. These rashes may burn or itch and can appear dark purple or brown on darker skin tones.
3. Neonatal Lupus
Neonatal lupus is a rare condition affecting newborns when certain antibodies are passed from the mother to the baby. Most symptoms resolve within six months, though heart problems may require ongoing treatment.
4. Drug-Induced Lupus
Drug-induced lupus is triggered by certain medications, including hydralazine, procainamide, and quinidine. Symptoms usually resolve after the medication is discontinued.
Blood Tests
While no single blood test can diagnose lupus, several tests provide important clues for an accurate diagnosis.
- Complete blood count: Measures levels of white blood cells, red blood cells, and platelets to assess overall blood health and detect anemia or other blood disorders
- Antinuclear antibody test (ANA): Detects autoantibodies that attack the body’s own cells; about 95 percent of people with lupus test positive for ANA, though 20 percent of healthy women may also have a positive result
- Complement test: Measures levels of complement proteins in the blood; low levels are often linked to lupus
Additional Tests
In addition to blood work, other diagnostic tests can provide important information about how lupus is affecting the body and help guide treatment decisions.
- Tissue biopsies: Examine a small sample of skin tissue under a microscope to help identify the cause of skin issues
- Urinalysis: Checks for elevated levels of blood or protein, which may indicate kidney involvement
- X-rays and scans: Assess potential organ damage when lupus is suspected to affect internal organs
- Echocardiogram: Examines the heart’s function and structure to help diagnose heart issues, including congenital heart block associated with neonatal lupus
1. Conventional Medicine
SLE
Commonly used medications for SLE include:
- NSAIDs: Over-the-counter medications such as ibuprofen and naproxen help ease mild joint and muscle pain, and reduce swelling
- Corticosteroids: Powerful medications reduce swelling, pain, and tenderness, and in higher doses, control the immune system; doctors aim for the lowest effective dose to limit side effects
- Antimalarial drugs: Medications such as hydroxychloroquine and chloroquine that help with joint pain, skin rashes, fatigue, and lung inflammation, and may help prevent lupus flares and extend lifespan
- Immunosuppressive agents: Medications used in severe cases affecting major organs that suppress the immune system but can cause serious side effects.
- Anifrolumab-FNIA: A type I interferon receptor antagonist used for moderate to severe SLE in adults
- Voclosporin: The only FDA-approved oral medication for lupus nephritis
- Biologic agents: Medications such as belimumab and rituximab specifically target pathways involved in lupus to help manage the disease
Skin Lupus
When treating skin lupus, dermatologists focus on clearing rashes, relieving pain and itching, preventing scarring, and addressing hair loss in discoid lupus. Treatment options include:
- Sun protection: Helps prevent flare-ups
- Medications such as corticosteroids, antimalarial drugs, and biologic agents: Also used to treat SLE
- Tacrolimus ointment: Used when corticosteroids are unsuitable
- Laser therapy: Helps treat persistent patches, dark spots, and scarring
People with cutaneous lupus typically visit their dermatologist every three to six months for ongoing care.
Neonatal Lupus
Treatment for neonatal lupus depends on specific symptoms:
- Topical steroids and sun protection to manage skin rashes
- Pacemaker placement for serious complications such as congenital heart block
Drug-Induced Lupus
Lupus-like symptoms typically resolve within six months after the medication is discontinued.
2. Traditional Chinese Medicine (TCM)
Some people with lupus explore complementary treatments such as TCM.
3. Supplements
Vitamin D supplementation is important for people with lupus, as they often need to avoid sunlight, which the body requires to produce vitamin D. Correcting a deficiency with supplements can support overall health, but evidence suggests omega-3 fatty acids may be more effective than vitamin D in reducing lupus activity, inflammation, and related symptoms.
1. Anti-Inflammation and Unprocessed Diet
While there is no specific “lupus diet,” maintaining a healthy, unprocessed diet is essential for managing lupus, as it can help regulate inflammation and manage common lupus-related symptoms.
- Fruits and vegetables, especially leafy greens
- Whole grains, beans, and nuts
- Lean meats, fatty fish, and eggs
Omega-3 fatty acids, particularly from fatty fish, may help reduce inflammation, oxidative stress, and fatigue while improving heart and mental health.
2. Low-Impact Exercise
Exercise—especially low-impact aerobic and resistance training—is an effective way to manage lupus symptoms by reducing inflammation, improving muscle flexibility, and boosting mental well-being. Activities such as walking or low to moderate-intensity aerobic exercise may help alleviate fatigue, depression, and other symptoms.
3. Mind-Body Interventions
Mind-body interventions, including mindfulness, relaxation techniques, and other behavioral approaches, may help reduce anxiety, depression, pain, and other lupus-related symptoms.
4. Sun Protection
Sun protection through clothing, sunscreen, and limiting sun exposure may help prevent flare-ups and skin damage. Many people with lupus are unaware of how ultraviolet radiation can worsen disease activity. However, reduced sun exposure may lead to vitamin D deficiency, making supplementation with vitamin D3 and K2 necessary for some people.
5. Sleep
Improving sleep quality is important, as sleep problems are common with lupus and can worsen fatigue, pain, depression, and other health issues.
6. Avoid Smoking
Smoking increases the risk of developing lupus and can worsen disease activity and outcomes.
Online Resources
While social media and general internet searches can be misleading, certain digital health resources may provide helpful information and support for people with lupus. Options to consider include:
- PatientsLikeMe
- Research Accelerated by You, associated with the Lupus Foundation of America
- OASH: Office of Women’s Health
- LUPUS UK Online Forum
- Lupus nephritis: A severe condition where the immune system attacks the kidneys, causing inflammation that can lead to kidney dysfunction or failure
- Accelerated atherosclerosis and coronary heart disease: Inflammation in the blood vessels that increases the risk of early-onset heart disease
- Neurological deficits: Cognitive dysfunction, headaches, seizures, or stroke that can result from lupus affecting the brain or nervous system
- Lupus vasculitis: Inflammation of the blood vessels that can affect multiple organs and lead to serious complications, depending on which vessels are involved
- Abnormal blood clotting: Overproduction of antibodies that can cause clotting disorders, leading to either excessive or inadequate clotting, sometimes persisting despite effective lupus treatment
- Anxiety and depression: Psychological symptoms that are common due to the physical and emotional toll of living with lupus
- Lung issues: Breathing problems such as pleuritis, pneumonia, pulmonary hypertension, or shrinking lung syndrome that can affect lung function and overall health
- Fibromyalgia: Chronic widespread pain that affects muscles and soft tissues and often co-occurs with lupus
- Infections: Increased vulnerability to bacterial and viral infections, such as urinary tract infections or cytomegalovirus, due to lupus and its treatments suppressing the immune system
- Macrophage activation syndrome: An overactive immune response that causes severe inflammation and symptoms resembling a lupus flare








