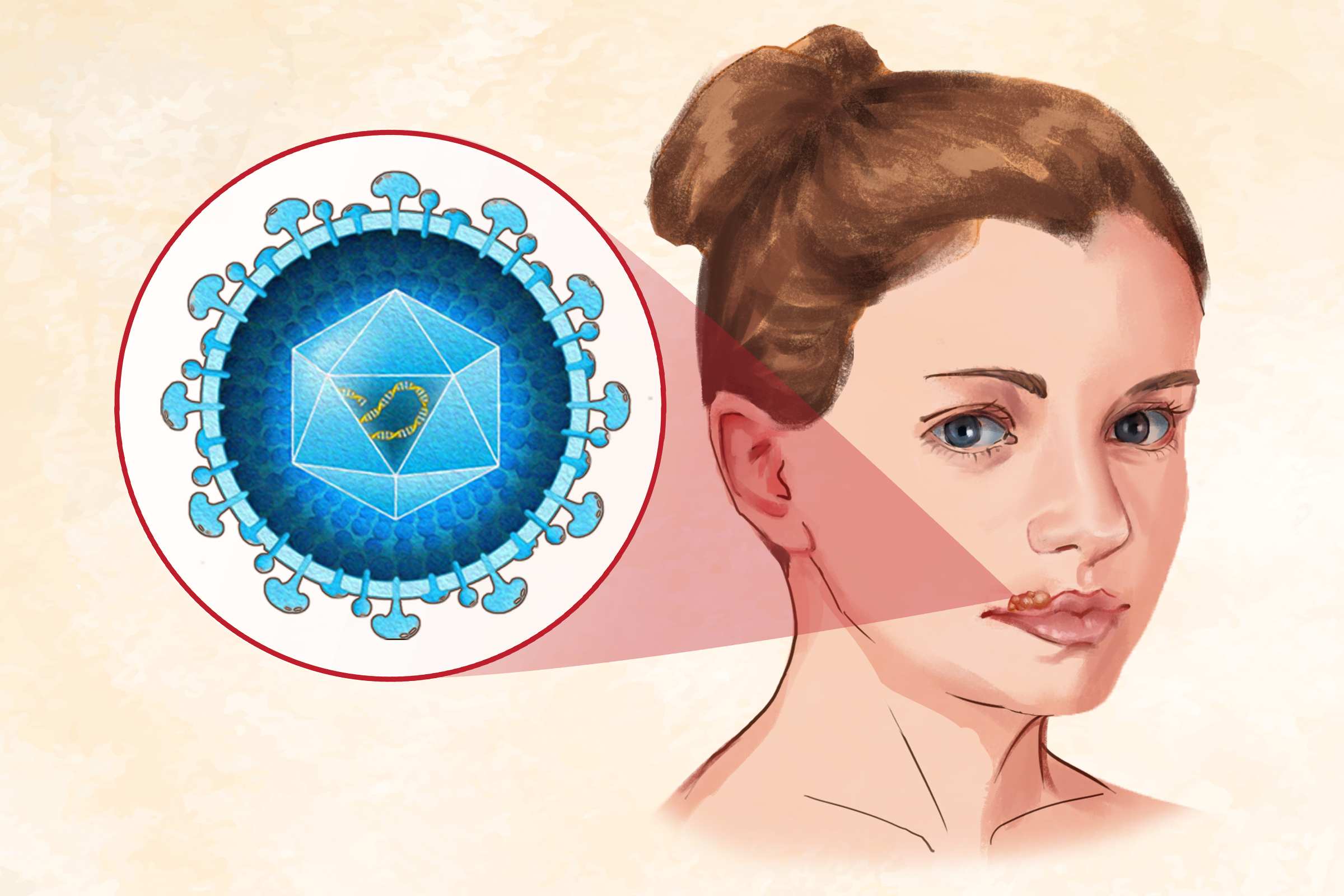
- Herpes simplex virus type 1 (HSV-1): HSV-1 causes both oral and genital herpes. It is primarily transmitted through oral contact, such as kissing or the exchange of saliva, causing infections in and around the mouth. Although it can be spread through sexual activities, oral herpes is usually not considered a sexually transmitted infection (STI). HSV-1 often causes herpetic gingivostomatitis, herpes labialis (cold sores), and herpes keratitis (herpes eye infection).
- Herpes simplex virus type 2 (HSV-2): HSV-2 also causes genital herpes and possibly oral herpes. Genital herpes caused by HSV-2 is significantly more likely to recur than genital herpes caused by HSV-1. HSV-2 is spread through sexual contact. Genital herpes is one of the most common STIs, although herpes virus infections often do not lead to severe disease. HSV-2 usually causes genital lesions, which are open sores and blisters.
Both HSV types can lead to painful blisters or ulcers that may recur over time.
- Early signs: If symptoms do emerge, they often start with tingling, itching, or burning near newly formed open sores and blisters or before sores and blisters emerge. Up to 50 percent of people with recurrent outbreaks experience such symptoms before sores and blisters develop.
- Oral herpes symptoms: Oral herpes symptoms usually start between three days and one week after exposure to the virus. Before sores appear, people might experience the following:
- Feeling unwell
- A reduced appetite
- A fever
- Swollen and tender lymph nodes
- General skin soreness
- A burning or tingling sensation around the infected areas
Sores typically form on the lips and around the mouth, starting as small blisters that can turn into pustules, open sores, and ulcers. Within 2 to 6 weeks, these sores usually crust over and heal, but they can come back. Recurring outbreaks are generally less severe than the first one. Sometimes, herpes can affect the hair follicles, causing a condition called herpetic sycosis, also known as HSV folliculitis, often linked to shaving closely with a razor.
- Genital herpes symptoms: Common symptoms of genital herpes include bumps, blisters, or open sores (ulcers) around the genitals or anus, as well as painful urination (especially for women). These sores and blisters are typically very painful and can be aggravated by friction, moisture, overheating, or certain types of clothing. Blisters may break open, ooze, and then crust over.
During their first herpes infection, people may also experience:
- Fever/flu-like symptoms
- Body aches
- Headache
- Nausea and vomiting
- Feeling of pressure in the abdomen
- Small red blisters or open sores—these symptoms typically affect the penis, foreskin, and scrotum in men and the labia, vagina, and cervix in women.
- Pain in the legs, buttocks, or genital area
- Swollen glands
- Unusual vaginal discharge
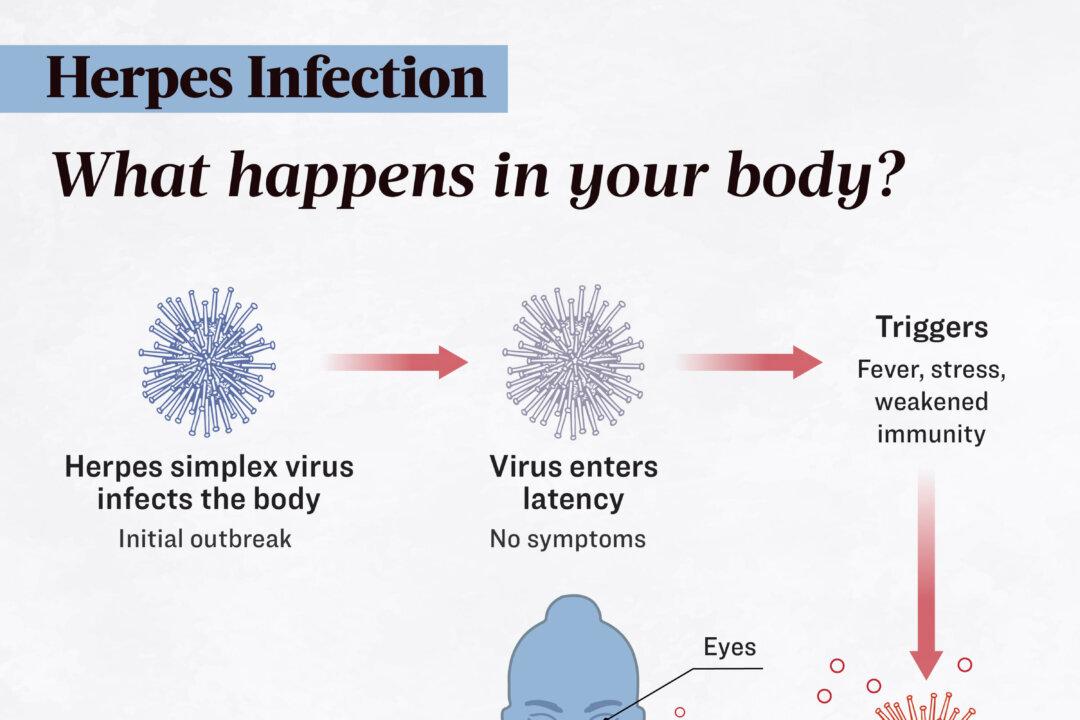
Genital herpes symptoms often recur in outbreaks. The first outbreak is usually the most severe, lasting two to three weeks, while future flare-ups are less severe and shorter. However, some people regularly shed (release infectious viral particles) the virus. Viral or bacterial infections, menstrual periods, and stress can potentially trigger outbreaks. Although genital herpes is a lifelong infection, the frequency of outbreaks may diminish over time.
1. How HSV-1 Spreads
HSV-1 is primarily spread through direct skin contact or contaminated saliva. HSV-1 is most transmissible through contact with sores, saliva, or surfaces around the mouth, especially during active outbreaks. Therefore, it can be contracted by kissing, sharing eating utensils or personal items such as razors, and receiving oral sex from someone with HSV-1. After infection, HSV-1 replicates at the infection site and travels to the dorsal root ganglia, where it becomes latent.
2. How HSV-2 Spreads
HSV-2 is usually transmitted during sex through contact with genital or anal surfaces, skin, sores, or fluids, and can spread even when no symptoms are present and the skin appears normal.
3. Mother-to-Child Transmission
Although most women with genital herpes give birth to healthy babies, in the United States, around 1 in 1,000 newborns contract neonatal herpes simplex virus, usually due to HSV exposure during vaginal delivery. Women with recurrent genital herpes have a low risk of passing the virus to their babies, but those who acquire genital HSV during pregnancy have a higher risk. Neonatal herpes typically appears between days 5 and 14 of life, affecting the scalp and trunk, and can cause cutaneous lesions, as well as infection of the oral and ocular mucosa. It may also impact the central nervous system, leading to symptoms such as encephalitis (brain inflammation), lethargy, poor feeding, bulging fontanelle (the soft spot on the baby’s skull), irritability, and seizures. The infection can be life-threatening to the child or result in brain damage.
- People under 50: According to the latest data, in 2016, approximately 3.7 billion people under 50, or 67 percent of the global population, were infected with HSV-1 (oral or genital). Most HSV-1 infections occur during childhood. Genital herpes caused by HSV-2 affected about 491 million people, or 13 percent of those aged 15 to 49 worldwide.
- Women: HSV-2 infects women nearly twice as often as men because the virus is more efficiently transmitted from men to women during sexual activity.
- Black women: Approximately 50 percent of African-American women between the ages of 14 and 49 are infected with HSV-2.
- Sexually active people: All sexually active individuals are at risk for genital herpes. Having multiple sexual partners furthers the risk.
- People who don’t practice safe sex: Not using condoms increases risk.
- Adolescents: The highest number of new infections occurs among adolescents.
- People with a weak immune system: People with HIV/AIDS or those on immunosuppressant drugs for autoimmune diseases or organ transplants are at a higher risk of severe cases of herpes.
- People who share personal items with others: Examples include drinking cups and cosmetics.
1. Differential Diagnosis
- Oral herpes: Conditions that can be confused with oral herpes include canker sores, Stevens-Johnson syndrome, erythema multiforme major, and herpangina (mouth blisters). These can be differentiated from oral herpes through medical history and physical examination.
- Genital herpes: Genital herpes share similar symptoms with conditions such as syphilis, chancroid, lymphogranuloma venereum, Crohn’s disease, Behcet syndrome, psoriasis, and sexual trauma.
2. Medical History and Physical Exam
Most doctors will review a person’s medical history and perform a physical examination before ordering tests. After the physical exam, tests can determine whether the infection is HSV-1 or HSV-2, which is important for effective long-term management.
3. Diagnostic Tests
Several tests are available to diagnose oral and genital herpes. They can be selected according to a patient’s symptoms. These tests include:
- HSV serology test: A serum herpes simplex antibodies test is a blood test that detects antibodies to HSV-1 and HSV-2. Antibodies are proteins produced by the body in response to an HSV infection. It shows whether someone has been infected with the herpes virus in the past, but it cannot determine when or from whom the infection occurred.
Antibodies may not be detectable during the initial infection period but will remain positive for life. This test can be useful for couples, especially if one partner has a history of genital herpes, as it helps in discussing prevention strategies if the other partner has not been infected. This serology test is considered the gold standard for diagnosing HSV-1. It is also useful when no symptoms are observed.
- Culture test: A culture test checks for the presence of the HSV in blisters or ulcers. It detects the virus in about 50 percent of people with genital ulcers and is more effective when the ulcers are new and open. Therefore, fluid and samples for culture should be collected from a freshly ulcerated lesion. The test is also more accurate during an initial herpes outbreak than during recurrent episodes.
- Polymerase chain reaction (PCR) test: The PCR test is a highly sensitive method for detecting the herpes virus in cells and secretions from the organs. It is more sensitive than the culture test.
- Biopsy: A biopsy for herpes involves taking a small tissue sample from a lesion or sore to be examined under a microscope. This helps confirm the HSV’s presence. The biopsy is usually performed when other tests are inconclusive or when there is a need to evaluate the severity of the infection.
- Direct immunofluorescence assay (DFA): The DFA is commonly used for the rapid identification of HSV infections in mucocutaneous lesions. It is an alternative to the HSV serology test.
- Tzanck smear: A Tzanck test involves scraping a fresh sore and using a special stain to check for giant cells with multiple nuclei, which indicates the presence of HSV. However, this test can only show that HSV is present and cannot differentiate between the different types of herpes virus.
- HIV infection: An HSV-2 infection can increase the risk of acquiring HIV by roughly three times and is considered a major complication of herpes. Individuals with both HIV and HSV-2 infections are more likely to transmit HIV to others.
- Encephalitis: This brain tissue infection is a severe complication of HSV-1 infection.
- Keratitis: Keratitis is the inflammation or irritation of the cornea. It is a rare complication of HSV-1 infection.
- Meningitis: Meningitis can be caused by an HSV-2 infection.
- Meningoencephalitis: When both the brain and meninges are infected, herpes meningoencephalitis is a medical emergency.
- Recurrent mouth sores and blisters: A complication of oral herpes
- Development of a bacterial skin infection: A complication of oral herpes
- Systemic body infection: This is potentially life-threatening in individuals with weakened immune systems due to conditions such as atopic dermatitis, cancer, or HIV infection.
- Proctitis: Proctitis is inflammation of the rectum or anus and can cause pain during defecation. This complication is more common among men who have sex with men.
- Acute retinal necrosis: Acute retinal necrosis typically presents with red eye(s), periorbital pain, and reduced vision. Examination shows episcleritis or scleritis, necrosis, and retinal detachment. It can occur with HSV-2 meningoencephalitis.
- Neurologic disability or death: These are severe complications of childhood and neonatal herpes.
- Vaginal yeast infections: A complication of genital herpes.
- Ongoing herpes infection with no periods of clear lesions
- Herpes infection in the esophagus
- Bladder issues causing difficulty with urination
- Herpes infection of the liver: This can result in cirrhosis (liver failure).
- Blindness: This is a rare complication of genital herpes.
- Lung infection
- Eczema herpeticum: Eczema herpeticum is a complication of HSV infection where severe herpes lesions develop on skin areas affected by eczema.
One can still have children despite having genital herpes. As aforementioned, HSV can be spread to an infant in the birth canal during delivery, causing neonatal herpes. The greatest risk for neonatal herpes is if a woman becomes infected with genital herpes late in pregnancy.
1. Medicines
Medicines are often used for both initial and recurrent herpes episodes.
- Antivirals: Symptomatic treatment with antivirals such as acyclovir, valacyclovir, or famciclovir is useful for initial herpes episodes and severe infections. Acyclovir is considered the gold standard therapy for HSV infections. It is usually well-tolerated, but possible side effects include inflammation of the veins, kidney issues, and, rarely, neurological problems such as lethargy, confusion, seizures, or coma, especially if kidney function is impaired.
Treatment may not be essential for later, less severe outbreaks. For instance, cold sores typically heal on their own within 2 to 3 weeks, but they can sometimes last up to 6 weeks. If antiviral medication is used, it generally requires a shorter duration of treatment. Treatment for recurrent herpes episodes is most effective if started within 48 hours of onset. Although early treatment can manage primary HSV infection, it does not prevent future recurrences. However, a daily low dose of these medications can help reduce the frequency of outbreaks. Acyclovir-resistant HSV infections are rare and typically occur in immunocompromised patients. In such cases, another FDA-approved antiviral, foscarnet, can be an effective treatment option.
- Antiviral topical ointments: Examples include acyclovir and penciclovir. For instance, applying topical penciclovir cream every two hours during waking hours for four days to the area affected by herpes labialis (cold sores) can help heal them faster and reduce symptoms. Over-the-counter creams with docosanol, applied five times a day, might also help provide some relief. However, topical ointments are usually less effective than oral antivirals, and they need to be administered multiple times a day.
- Intravenous antivirals: Severe HSV infections, such as herpes encephalitis and infections in newborns, are treated with intravenous acyclovir.
- Painkillers: If genital herpes is causing severe pain, painkillers can provide relief.
- Over-the-counter topical anesthetics or anti-inflammatory agents: These can be used to reduce herpes symptoms. Applying topical anesthetics such as benzocaine can help relieve pain from sores. For multiple sores in the mouth, rinsing with lidocaine may be effective. These anesthetics should not be swallowed and should only be used as directed to avoid harmful side effects.
For genital herpes, there are two types of therapy involving antiviral medications:
- Episodic therapy: This approach involves taking antiviral medications only during outbreaks, and is suitable for individuals with fewer than six outbreaks per year. It helps reduce the duration and severity of symptoms if started within 72 hours of the first herpes signs. However, episodic therapy does not decrease the frequency of outbreaks. It is useful for managing symptoms more effectively when outbreaks occur.
- Suppressive therapy: This involves daily antiviral medication to prevent outbreaks and reduce their frequency and duration. It also lowers the risk of transmitting HSV to an uninfected partner. It is recommended for those with six or more outbreaks per year, a weakened immune system, or when in a relationship with an uninfected partner. Suppressive therapy can reduce transmission risk by about 50 percent. The duration of suppressive therapy is uncertain, and periodic breaks may be suggested to reassess the need for continued treatment.
Herpes medications generally have very few side effects and no major complications. However, they may be less effective in people with severe immunosuppression or those who have been using them for a long time. Some individuals might require higher doses to control their outbreaks.
2. Home Remedies
- During outbreaks: You can speed healing and prevent spreading herpes by keeping sores clean and dry, avoiding touching them, washing your hands after any contact, and refraining from sexual contact until the sores are healed.
- Avoid sun exposure: For individuals whose oral herpes outbreaks are triggered by sunlight, avoiding sun exposure and using sunscreen can help reduce the risk of recurrences.
- Cold drinks: To alleviate symptoms of oral herpes, individuals can drink plenty of cold beverages and eat popsicles.
- Warm baths: To relieve symptoms of genital herpes, individuals can bathe in a warm, soap-free bath and wear loose-fitting clothing to minimize skin irritation and moisture buildup.
- Ice or warm compresses
1. Medicinal Herbs
- Traditional Chinese herbal medicines: In vitro studies have shown that several Chinese herbal medicines exhibited stronger anti-HSV-1 activity when combined with acyclovir, compared to other herbal extracts. They are:
- Geum japonicum: Commonly known as Asian herb bennet, Geum japonicum is often used to relieve dizziness and headaches.
- Rhus javanica: In guinea pigs infected with HSV type 2, oral administration of Rhus javanica significantly reduced the incidence, severity, and frequency of genital herpes lesions compared to those receiving water.
- Clove (Syzygium aromaticum)
- Terminalia chebula: Known as the “king of medicine” in Tibet, Terminalia chebula is highly revered in the Ayurvedic medical system due to its exceptional healing abilities.
- Antrodia camphorata: In a 2016 study, Antrodia camphorata, a traditional Chinese medicinal mushroom used for liver diseases and cancers, exhibited the ability to inhibit HSV replication at very low concentrations. Its bioactive compound antrodin A also reduces viral spread between cells.
- Murici (Byrsonima verbascifolia): A 2001 study found 13 plant extracts effective against HSV, with Byrsonima verbascifolia showing the strongest activity at a concentration as low as 2.5 micrograms per milliliter. Byrsonima verbascifolia, commonly known as murici in Brazil, is a medicinal plant widely used to treat bacterial and viral infections, bronchitis, cough, fever, and many other diseases.
- Siberian ginseng (Eleutherococcus senticosus): Also called eleuthero, Siberian ginseng is distinct from American and Asian ginseng. Its active ingredients, eleutherosides, may help stimulate the immune system. One study involving 93 people with HSV-2 infection found that Siberian ginseng reduced the number and severity of genital herpes outbreaks, and shortened their duration.
2. Dietary Supplements
- Lysine: Lysine, also known as L-lysine, is an essential amino acid. In an early study, participants took lysine monohydrochloride tablets (1,000 milligrams per dose) three times daily for six months. The treatment was found to effectively reduce the frequency, severity, and healing time of recurrent HSV infections.
- Zinc: A 2020 study found that zinc deficiency could prolong cold sores caused by HSV. The topical use of low concentrations of zinc (0.025 to 0.05 percent) was also shown to be effective in treating oral and genital herpes outbreaks.
3. Essential Oils
According to a review in Chemotherapy, many essential oils and their ingredients can destroy or inactivate both types of HSV directly and hinder or prevent the viruses’ multiplication inside cells.
- Peppermint oil: Peppermint oil, the essential oil of Mentha piperita, has shown strong antiviral effects in in vitro studies. Peppermint oil is generally considered safe when taken orally or applied topically in common doses.
- Clove essential oil: Eugenol, a key component of clove oil, was tested for its antiviral effects against HSV-1 and HSV-2 and found to inhibit virus replication in lab tests. Eugenol combined with acyclovir enhanced antiviral effects, and its topical application delayed herpes-induced keratitis in mice.
- Tee tree oil: A 2001 study found Australian tea tree oil to be highly effective against both HSV-1 and HSV-2 in cell cultures. At safe concentrations, it reduced the growth of the virus by 98.2 percent for HSV-1 and 93.0 percent for HSV-2. The potential use of tea tree oil as an antiviral agent in treating recurrent herpes infection showed promise, according to the study, though the active components responsible for their anti-herpes properties were not identified.
4. Apitherapy
A 2019 systematic review examined three clinical trials on the effects of honey and six of propolis on herpes infection. The trials demonstrated that both bee products have potential as alternatives to acyclovir in treating herpetic skin lesions. Propolis, in particular, was found to be superior to acyclovir in four of the trials. This suggests that propolis may be the most effective natural option for treating herpetic lesions, especially those related to HSV-1.
5. Diet
Including immune system-boosting foods in your diet may help prevent herpes outbreaks and accelerate healing:
- Antioxidant-rich veggies: such as spinach, kale, and tomatoes, can help reduce oxidative stress in the body.
- Fruits and vegetables rich in vitamin C: such as berries, citrus, red peppers, and cruciferous vegetables.
- Zinc-rich foods: Such foods include meat and seafood.
- Foods rich in vitamin B12: Vitamin B12 can help regulate your immune system, making it more effective at fighting viral infections.
- Stress management: High levels of stress can trigger or exacerbate herpes outbreaks. A proactive mindset can enhance coping strategies and stress management techniques, such as mindfulness, relaxation exercises, and adequate sleep, thus helping reduce the frequency and severity of outbreaks.
- Emotional well-being: Individuals diagnosed with genital herpes may exhibit various reactions, including strong emotions and anxiety due to personal perceptions and stigma, with common psychological responses being shame, guilt, and anger. These emotions can discourage them from seeking further care, disclosing their infection status to partners, or fully participating in their daily lives. A positive mindset can make herpes patients more receptive to counseling, therapy, and support groups, which can help them manage their emotional aspects of living with herpes, potentially reducing the physical impact of the virus as well.
- Adherence to treatment: A positive mindset about managing herpes and adhering to prescribed treatments can improve physical outcomes. Believing in the effectiveness of treatment can lead to better adherence and more consistent management of the condition.
- Self-care and prevention: A proactive attitude towards self-care, including practicing good hygiene, using medications as prescribed, and avoiding triggers, can help reduce the risk of outbreaks and transmission.
- To prevent the spread of oral herpes, avoid oral contact with others and refrain from sharing items that have come into contact with saliva.
- To prevent the spread of genital herpes refrain from sexual activity (vaginal, anal, and oral sex). Even without herpes symptoms, others can be infected through viral shedding. People with genital herpes are advised to avoid sex at the first sign of an outbreak, as the risk of transmitting the virus is highest during that time.
- Inform sexual partners of herpes status to help reduce the risk of transmission.
- If individuals with herpes have sexual activities, using condoms and dental dams can reduce the risk of spreading and getting an STI. Birth control methods, such as pills or implants, do not protect against STIs.
- Past, current, and future partners of an individual with herpes might benefit from evaluation and HSV type-specific serologic testing to help prevent neonatal herpes.
- Adhere to treatment to reduce outbreaks and their severity. Treating an infected partner with suppressive therapy can prevent the transmission of symptomatic herpes to an uninfected partner in over 90 percent of cases.
- If a pregnant mother is infected with genital herpes, cesarean delivery is recommended to prevent transmission to the newborn. Fetal scalp monitors should also be avoided during labor.
To prevent oral and genital herpes or reduce the risk of infection, you can do the following:
- Avoid sharing silverware, glasses, straws, lip balm, or other items with someone who has oral herpes.
- Stay in a long-term monogamous relationship with a partner who does not have herpes.
- Practice safe sex, such as using a condom. However, condoms may not fully protect against herpes, because not all sores occur in areas a condom covers, and the virus can be shed from skin without visible sores.
- Limit your number of intimate partners.
- Avoid douching, as it removes beneficial bacteria in the vagina that help protect against infections.
- Learn about a potential intimate partner’s STI status.
- Avoid alcohol or drug abuse, as excessive use can lead to risky behavior.
Mothers with genital herpes can still breastfeed as long as they do not have herpes sores on their breasts. If they have sores on one or both breasts, they should avoid breastfeeding directly from the affected breast. Instead, they can pump or hand-express milk from that breast until the sores heal, while ensuring that neither their baby nor pumping equipment comes into contact with the sores.