Symptoms
Fibromyalgia presents with a wide range of symptoms, but certain ones appear more consistently and can significantly interfere with daily life. These primary symptoms often serve as key indicators for diagnosis and management.
- Widespread pain: The hallmark symptom involves chronic pain in muscles, ligaments, and tendons. Pain can range from mild to severe and often worsens with activity, cold weather, or stress. It may feel like burning.
- Stiffness: Commonly felt in the morning, often improving during the day but returning or worsening at night.
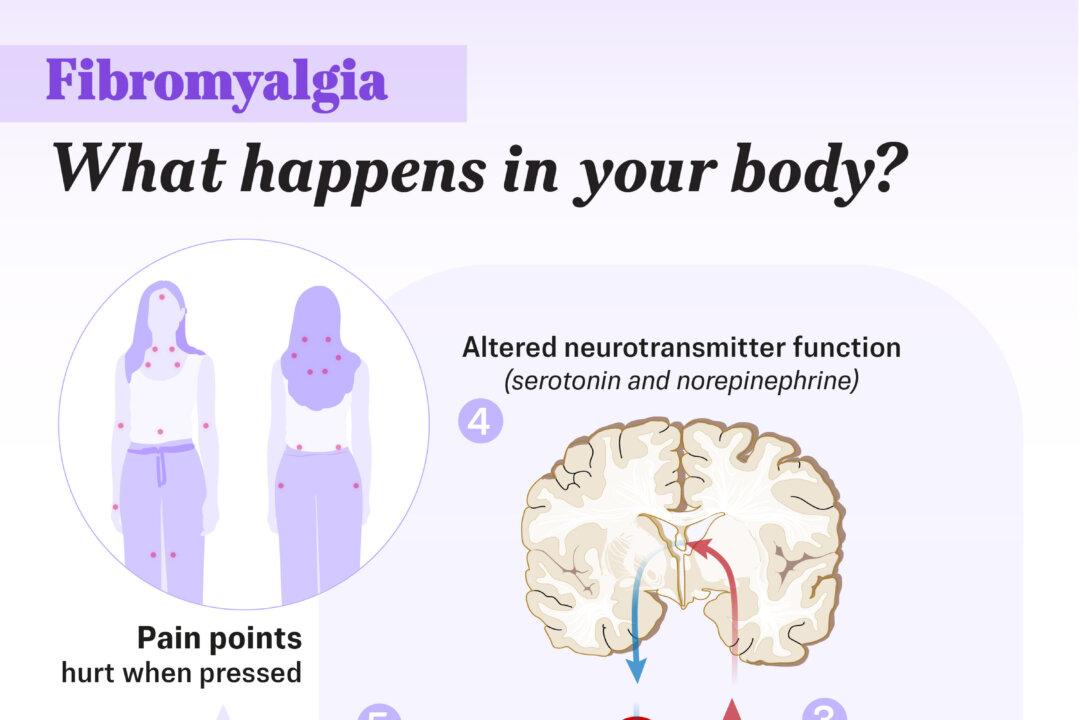
- Tender points: Also called trigger points, these are specific, sensitive areas on the body—18 in total—that hurt when pressed. The pain may radiate to other areas. Even a friendly hug can cause intense pain.
- Increased sensitivity to sensory stimuli: Includes heightened reaction to temperature, light, sound, and smell.
- “Fibro fog”: Also known as “brain fog,” this involves cognitive issues such as memory lapses, trouble concentrating, mental confusion, and slow thinking.
- Extreme fatigue: Persistent tiredness that does not improve with sleep—sometimes more debilitating than the pain itself.
- Headaches: More than half of people with fibromyalgia experience frequent headaches, including migraines and tension-type headaches.
- Sleep disorders: Nonrestorative sleep caused by conditions such as insomnia, sleep apnea, and restless legs syndrome. Many people wake up feeling unrefreshed despite 8 to 10 hours of sleep.
- Other symptoms: May include an overactive bladder, decreased exercise endurance, dry eyes, and digestive problems such as irritable bowel syndrome, constipation, and diarrhea. Women with fibromyalgia may experience more severe menstrual pain.
Mental health issues such as anxiety and depression are also common.
Symptom Flares
People with fibromyalgia often experience fluctuating symptoms, including periods known as “flares,” when symptoms become more intense. Flares are commonly triggered by stress-related factors such as illness, travel, weather changes, hormonal shifts, medication adjustments, or emotionally stressful situations.
- Genetics: A family history increases the risk; people with a close relative who has fibromyalgia are more likely to develop the condition.
- Immunity and inflammation: Elevated inflammatory cytokines and neurogenic inflammation in the brain, spinal cord, and peripheral tissues may play a role.
- Environmental triggers: Physical trauma such as car accidents or surgery; painful conditions like acute diseases; infections, including Lyme disease or COVID-19. Emotional trauma, including post-traumatic stress disorder, may also trigger fibromyalgia.
Additional risk factors:
- Gender: Women are twice as likely as men to develop fibromyalgia. Hormonal fluctuations, higher anxiety levels, and increased pain sensitivity may contribute.
- Age: Fibromyalgia often begins in midlife, with risk increasing with age. It is most commonly diagnosed in people between the ages of 35 and 45.
- Obesity: Obesity is associated with a higher risk of fibromyalgia and more severe symptoms. Inflammation associated with obesity may further worsen pain.
Most cases arise spontaneously, without an identifiable underlying medical condition. In other cases, fibromyalgia occurs alongside chronic health conditions such as rheumatoid arthritis, lupus, ankylosing spondylitis, osteoarthritis, as well as conditions like chronic back pain, irritable bowel syndrome, sleep disorders, depression, and anxiety. In such cases, fibromyalgia symptoms may overlap or be triggered by the primary illness, making diagnosis and management more complex.
- A widespread pain index (WPI) score of seven or higher and a symptom severity (SS) score of five or more, or a WPI of three to six and an SS score of nine or higher
- Symptoms present at a consistent level for at least three months
- No other medical condition that could explain the symptoms
The WPI assesses how many areas of the body are painful, while the SS scale evaluates fatigue, unrefreshing sleep, and cognitive difficulties.
1. Medical History Review
The doctor will ask about your symptoms—including the location, intensity, and duration of pain, fatigue, and cognitive problems—and inquire about any family history of fibromyalgia or related conditions.
2. Physical Examination
A physical exam can help rule out other conditions with similar symptoms, such as chronic fatigue syndrome, myofascial pain syndrome, polymyalgia rheumatica, or multiple sclerosis.
3. Diagnostic Testing
Lab work and imaging tests may be ordered—not to detect fibromyalgia directly, but to exclude other causes of pain. These tests may include:
- Blood tests: A complete blood count, C-reactive protein test, thyroid function tests, and other labs may be used to detect inflammation, hormonal imbalances, or related health conditions.
- Urine tests: Used to identify abnormalities that may suggest other underlying disorders.
- Imaging tests (such as X-rays): Used to rule out structural problems or diseases that could cause similar symptoms.
1. Anti-Inflammatory and Trigger-Free Diet
Eating anti-inflammatory foods—such as leafy green and dark yellow vegetables, fruits, and whole grains—may help ease pain and inflammation associated with fibromyalgia.
2. Supplements
Several supplements may help manage symptoms:
- Magnesium: A 2022 study found that magnesium supplementation may reduce stress and pain. Research suggests that 300 milligrams of magnesium citrate daily may improve tender points, depression, and anxiety.
- Vitamin D: Supplementation may help reduce fibromyalgia pain in people with low vitamin D levels.
- Acetyl L-Carnitine (ALCAR): A 2015 study indicated ALCAR may reduce pain and depressive symptoms while improving quality of life.
- S-Adenosylmethionine: Taking 800 milligrams daily may help reduce pain, morning stiffness, fatigue, and mood-related symptoms.
- Coenzyme Q10: A 2021 study found that taking 300 milligrams daily for 40 days significantly reduced pain, tender points, fatigue, and morning tiredness.
- Melatonin: Supplementation may help reduce pain, increase pain threshold, and improve sleep quality.
3. Stress Management
Tai chi and qigong are traditional Chinese practices that combine gentle movement, breathing, and meditation to promote relaxation and overall well-being.
4. Sleep Hygiene
Aim for 7 to 8 hours of quality sleep each night by following these strategies:
- Maintain consistent bedtime and wake-up times
- Avoid caffeine, alcohol, and spicy foods before bed
- Limit or eliminate daytime naps
- Engage in calming activities before sleep
5. Smoking Cessation
Among people with fibromyalgia, smoking is associated with cognitive dysfunction, more severe symptoms, lower quality of life, sleep problems, and increased anxiety compared to nonsmokers. Quitting smoking is an important step toward symptom relief.
1. Medications
There are three FDA-approved medications for fibromyalgia: duloxetine, milnacipran, and pregabalin. In general, medications that may help with fibromyalgia include:
- Antidepressants: Duloxetine and milnacipran are classified as serotonin and norepinephrine reuptake inhibitors. These medications increase levels of these neurotransmitters in the brain, which may reduce pain sensitivity and improve fatigue. Antidepressants can cause serious side effects, including suicidal thoughts—particularly in children and young people—though these effects are uncommon.
- Anticonvulsants: Pregabalin is approved to treat fibromyalgia and functions by calming overactive nerve cells involved in pain signaling. It may also improve sleep quality, which is often disrupted in people with fibromyalgia.
- Analgesics: Acetaminophen and nonsteroidal anti-inflammatory drugs—including ibuprofen and naproxen—may offer temporary relief for some people. However, major clinical guidelines do not recommend them due to limited effectiveness and potential side effects.
- Muscle relaxants: Cyclobenzaprine may be prescribed to reduce pain and support restful sleep. Other muscle relaxants have not been shown to be effective for fibromyalgia.
2. Talk Therapy and Counseling
Psychotherapy, or talk therapy, includes various approaches that help people manage pain, stress, and emotional challenges by addressing harmful thought patterns and behaviors.
3. Hyperbaric Oxygen Therapy (HBOT)
HBOT involves breathing pure oxygen in a pressurized chamber to enhance the body’s healing process. A 2023 study found that HBOT was significantly more effective than pregabalin and duloxetine in reducing pain in people with fibromyalgia.
4. Transcranial Direct Current Stimulation (tDCS)
tDCS is a noninvasive brain stimulation technique that alters brain activity to influence mood and behavior. A 2023 meta-analysis found that tDCS provided short-term pain relief and short- to mid-term improvements in depression and anxiety among people with fibromyalgia.
5. Low-Impact Exercises
Physical therapy, which uses movement-based treatments to restore function and mobility, plays a key role in fibromyalgia care.
6. Integrative Therapies
Complementary and integrative therapies may offer relief from fibromyalgia symptoms when used alongside conventional care. These approaches aim to support the mind-body connection, reduce stress, and ease physical discomfort.
- Acupuncture: A 2019 meta-analysis of 12 studies found that acupuncture appears to be a safe and effective treatment for people with fibromyalgia.
- Topical capsaicin therapy: A randomized controlled study involving 130 people found that those who received topical capsaicin experienced symptom improvement after six weeks.
- Massage: A 2014 meta-analysis found that massage therapy, when administered for at least five weeks, provided immediate relief in reducing pain, anxiety, and depression.
- Mindfulness practice: A 2016 study found that people with fibromyalgia who completed a Mindfulness-Based Stress Reduction program reported significant improvements in perceived stress, sleep quality, and overall symptom severity.
- Increased likelihood of hospitalization—people with fibromyalgia are twice as likely to be hospitalized
- Reduced quality of life
- Coexistence with other rheumatic conditions, including lupus, osteoarthritis, and rheumatoid arthritis
- Higher risk of major depression—adults with fibromyalgia are more than three times as likely to experience it
- Elevated risk of suicide and injury-related deaths
- Stable overall mortality rate—despite these risks, life expectancy remains similar to that of the general population