A new study published in Cell Metabolism found that chemicals released by intestinal microbes can be captured from breath and used to identify the bacteria living in a child’s gut. When researchers tested children with asthma, they found the breath analysis could predict the presence of Eubacterium siraeum, a specific bacterium associated with the respiratory condition.
“The data is very promising and exciting, especially if it can lead to improvement in care of patients with common childhood disorders such as asthma,” Dr. Pradnya Mitroo, a board-certified gastroenterologist and president and CEO of Fresno Digestive Health, who was not involved in the study, told The Epoch Times.
How the Test Works
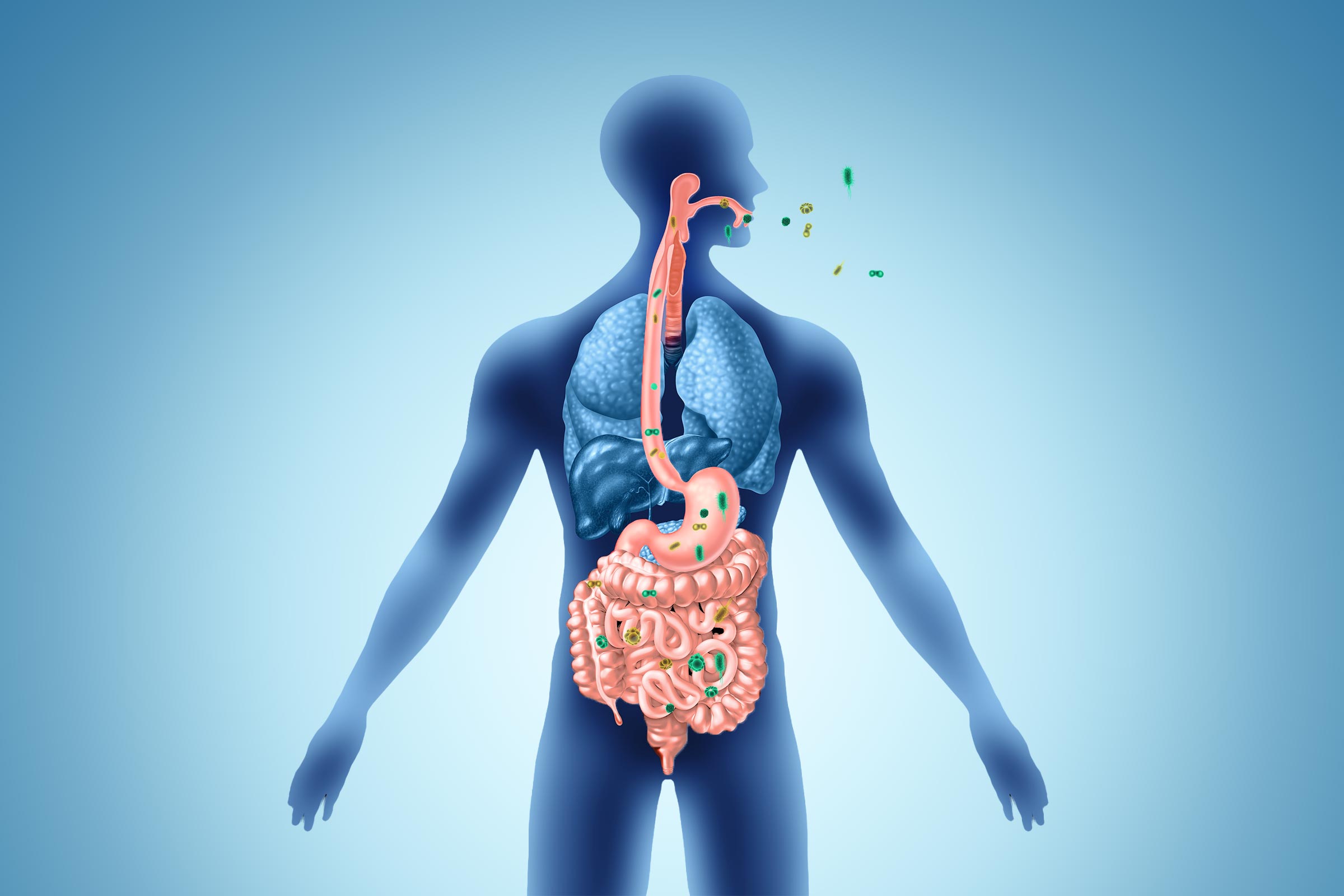
The team from Washington University School of Medicine in St. Louis and Children’s Hospital of Philadelphia analyzed breath and stool samples from 27 healthy children ages 6 to 12. They found that volatile organic compounds—chemicals that microbes release when digesting food—travel from the gut into the bloodstream and are eventually exhaled in breath.
The compounds detected in the breath matched those produced by the microbes in the children’s stool.
Similar results were seen in animal studies, in which gut bacteria were transplanted into microbe-free mice, and the breath compounds accurately indicated the presence of the bacteria.
When comparing samples from children with asthma with those from healthy children, researchers found that children with asthma had more abundant levels of Eubacterium siraeum. The breath test successfully predicted the presence of this bacterium, potentially offering a way to identify early microbiome changes that may worsen asthma symptoms.
Disruptions of the gut microbiome have been associated with several gastrointestinal conditions, including irritable bowel syndrome and inflammatory bowel disease, Dr. Sherin Daniel, director of pediatric gastroenterology at Northwell Health Staten Island University Hospital, who was not involved in the study, told The Epoch Times.
“Diagnosing children can be challenging, as they may not always be able to clearly describe their symptoms,” she said. “If validated for clinical use, this technology could allow us to gather meaningful clinical information with far less burden on patients and families.”
Clinical Applications
“Rapid assessment of the gut microbiome’s health could significantly enhance clinical care, especially for young children,” senior study author Dr. Andrew L. Kau, an associate professor at WashU Medicine, said in a press statement.
“Early detection could lead to prompt interventions for conditions like allergies and serious bacterial infections in preterm infants,” he added, emphasizing that the study “lays the groundwork” for developing this type of diagnostic tool.
Such breath tests could be useful in detecting microbiome disruptions in infants born prematurely, potentially spotting infections before symptoms develop.
“Breath analysis offers a promising, noninvasive way to probe the gut microbiome and can transform how we diagnose disease in medicine,” first author Ariel J. Hernandez-Leyva, a medical and doctoral student at WashU Medicine, stated in the press statement.
He added that the study findings may lead to the development of a simple device that diagnoses gut health issues just by breathing into it—similar to previous breath tests developed by the same research team for detecting COVID-19 in less than a minute.
Advantages of Breath Testing
Gastroenterologists not involved in the study noted that the approach addresses real-world barriers to pediatric care.
Compared with current diagnostic methods, such as medical histories, physical examinations, and laboratory tests, a breath test is fast, painless, and far more child-friendly, Mitroo said. The real advantage, she added, is repeatability.
“You could track gut health over time very easily [by] measuring these compounds with a breath test rather than asking families to collect [stool] samples or undergo procedures,” Mitroo added.
Parents don’t need advanced testing to know when something is off. Persistent abdominal pain, changes in bowel habits or blood in the stool, poor growth, or symptoms that wake a child at night should prompt evaluation, she noted.
Breathing into a device is “far less intimidating” than blood draws, stool collection, or invasive testing such as endoscopy, which involves an optical probe, Dr. Jason Korenblit, a gastroenterologist and digestive health expert at JustAnswer, who was not involved in the study, told The Epoch Times. “That matters a lot for children, anxious patients, and families juggling school and work,” he said.
“If the goal is to monitor change over time—such as after antibiotics, diet changes, new symptoms, or treatment—patients are more likely to follow through with a quick breath sample than repeated stool kits,” Korenblit added.
A noninvasive, rapid way to assess microbial activity could move gut health from “theory into everyday care—especially for children,” Mitroo said, noting that such a test still shouldn’t replace a doctor’s clinical judgment.
“That said, this is early research,” she said. “We need larger studies and proof that acting on these signals actually improves outcomes for patients.”
While the technology shows promise, experts emphasized that it remains in the early stages. The initial study involved only 27 children, and larger clinical trials are needed to validate the approach and demonstrate that acting on breath test results actually improves patient outcomes.
Larger studies and clinical validation will be needed before this becomes part of routine practice, Daniel said, “but the potential impact on how we evaluate and follow children with gastrointestinal and immune-related conditions is evolving and very promising.”