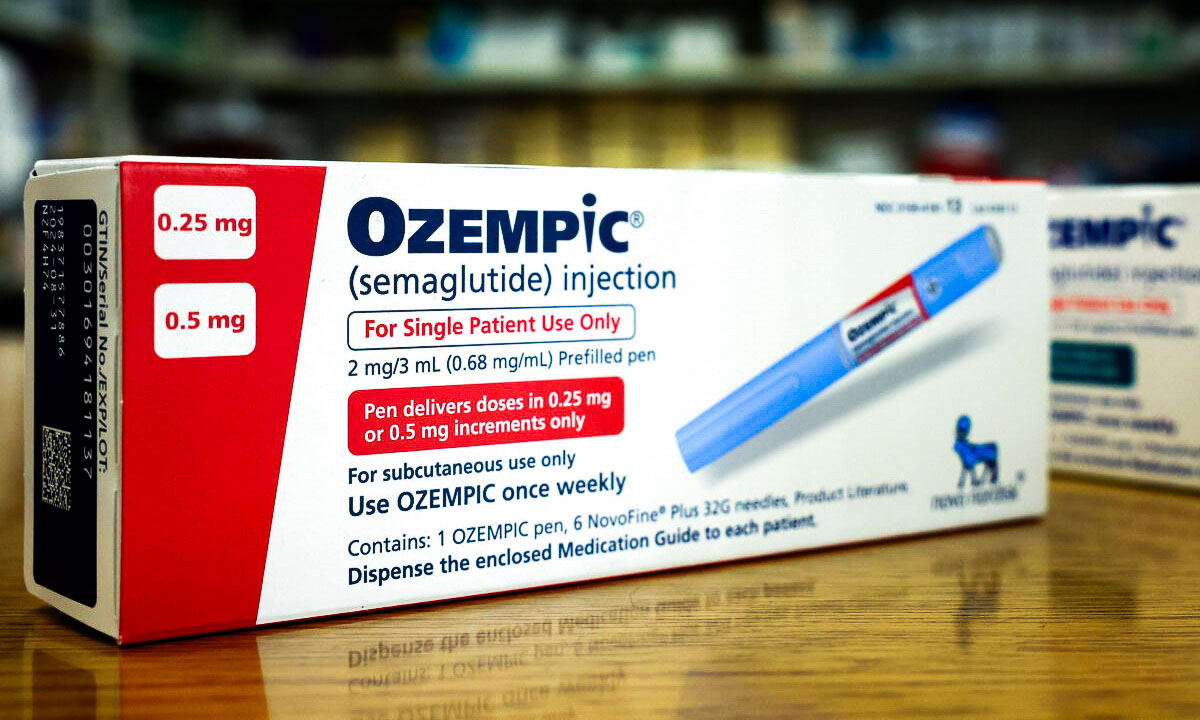
Popular weight loss medications such as Ozempic and Mounjaro could offer an unexpected weapon against the United States’ deadly opioid epidemic, with new research showing that patients taking these drugs were 40 percent less likely to be hospitalized for drug overdoses and 50 percent less likely to require treatment for alcohol intoxication.
The findings, published in the journal Addiction, represent a potential breakthrough in addiction treatment at a critical moment.
As drug overdose deaths have surged to record levels—increasing sixfold since 1999—medical researchers are looking to find new tools to combat substance abuse disorders.
While the study was observational and can’t prove direct causation, the reduction in hospitalizations among patients taking GLP-1 drugs such as semaglutide suggests that these medications, already affecting obesity treatment, could offer a new approach to addiction medicine.
Much Less Likely to Be Hospitalized for Overdose or Intoxication
Researchers analyzed real-world data from more than 500,000 patients with opioid use disorder (OUD) and 800,000 with alcohol use disorder (AUD) who were prescribed GIP or GLP-1 receptor agonist drugs such as Ozempic (semaglutide) and Mounjaro (tirzepatide).The study found that participants taking these drugs had 40 percent lower rates of opioid overdose and 50 percent lower rates of alcohol intoxication than those not taking the medications. Even when looking at different health conditions, patients with OUD and AUD who received GIP/GLP-1 RA prescriptions still showed lower rates of both opioid overdoses and alcohol intoxication.
These results are consistent with animal studies showing that GLP-1 RA drugs can reduce substance-related behaviors in rodents, the authors wrote.
“This study suggests that patients with heroin or alcohol addiction who are prescribed Ozempic (typically for diabetes or obesity) are less likely to be hospitalized for heroin overdose or alcohol intoxication, respectively,” Matt Field, professor of psychology at the University of Sheffield, who was not involved in the study, said in a statement.
However, he cautioned that the study focused on “very extreme” cases of substance intoxication, rather than the more common metrics used in addiction treatment research. Traditional addiction studies examine whether treatments help people achieve complete abstinence or reduce their substance consumption and frequency of use, Field added.
The researchers emphasized that their findings, while based on observational data that cannot prove direct causation, suggest a promising avenue for treatment. They called for prospective clinical trials to validate these associations and understand the underlying mechanisms.
They added that the results of the new study should encourage additional research into the potential benefits of Ozempic and related medications in addressing substance use disorders.