Sofia never really felt like she fit in as a preteen, so she turned to a place where she could get lost and go numb.
She sat scrolling on her smartphone, hour after hour, day after day, searching for her identity. It was an easy distraction from the social isolation of the COVID-19 pandemic quarantine and the pain of her parents’ divorce.
“I was so enraptured by what was going on in my phone,” Sofia, now 15, told The Epoch Times. Caught up in standards that she didn’t think she could achieve, she hated herself and was genuinely terrified by the thought of talking to peers.
“After quarantine, I would go out, I’d be profusely sweating,” she said. “I would be nervous, my face would be burning when I was talking to people.”
Rather than discuss her feelings, she would let them build up inside until she exploded with emotion.

Sofia, now 15, fell into the pitfalls of social media as a preteen. (Courtesy of Sofia)
Sofia considered her options. She watched peers brag about anxiety medications on social media and saw them isolating further into unchecked phone scrolling. Like Sofia, today’s teens are prone to the trap of social media, which encourages anxiety and depression and grooms them to believe that medication is the only way to escape the uncomfortable—and sometimes normal—feelings that accompany adolescence.
Platforms such as TikTok have amplified a broad spectrum of voices around drugs for teen anxiety and depression. Those voices include psychiatrists educating about various medications, influencers creating sponsored content, pharmaceutical companies posting advertisements, and even teens boasting about their own anti-anxiety prescriptions.
Teen Anxiety Then and Now
Today’s barrage of medicalized anxiety messaging sharply contrasts with the messaging two generations ago, when selective serotonin reuptake inhibitor (SSRI) drugs were first hitting the market for depression and anxiety. Drugs were then a relatively unfamiliar—and often private—solution for mental health struggles.
Social media has brought more awareness and normalization to teen mental health issues. However, experts are concerned that lopsided attention given to the quick fix of medication interferes with efforts to prevent anxiety and depression and holistic approaches to dealing with mental health.
Research shows that risks associated with anti-anxiety and antidepressant medications—such as drug dependence and tolerance, as well as overdosing and suicide—are rising among teens while therapy is becoming less common.
“In the United States, there’s so much advertising from drug companies that talk about mental health problems,“ Dr. Josef Witt-Doerring, a board-certified psychiatrist who specializes in treating adverse effects from psychiatric drugs, told The Epoch Times. ”So teens are less likely to see anxiety as an understandable response to stress and more like a physical problem.
“Because of that, they either get prescribed medications by the doctors, or they actually go to doctors and say: ‘There’s something wrong with me. I need medication.' And this is also amplified on social media.”
Witt-Doerring noted that anxiety is especially normal for teens and young adults who are in the midst of life transitions.
Yet teens are especially prone to a preconceived notion that they have a chemical imbalance in their brains, he said. There is no test that can accurately assess neurotransmitter levels related to depression and anxiety, and no evidence that drugs fix imbalances, Witt-Doerring said.
Algorithm Aggravations
A survey by Education Week, a publication for educators, found widespread evidence of teens using social media as a platform to diagnose their own and their peers’ mental health conditions.
The survey found:
- Sixty-five percent of school leaders and teachers reported that students sometimes or frequently use social media to diagnose their own mental health conditions.
- Fifty-five percent of high school students admitted to using social media to diagnose their own mental health conditions at least once, 28 percent said they do it sometimes, and 10 percent said they do it all of the time.
Nearly half of TikTok’s most viewed content revolves around poor mental health and includes mental health hashtags, according to a European Child and Adolescent Psychiatry systematic
review.
It found that trending mental health topics—tics, dissociative identity disorder, and self-harm in particular—were associated with an uptick in treatment for those conditions.
TikTok has made it a badge of honor for teen users to belong to a community of other teens and celebrities who struggle with anxiety and depression, Witt-Doerring said.
“There’s a lot of content out there with people saying, ‘This is a day in the life of someone with major depressive disorder, and here are all the drugs that I’m taking,’” he said. “And it really normalizes it for people. You see it enough times and you’re just like, ‘Oh, I guess everyone has these brain diseases, and they need to be on all these drugs.’”
TikTok did not respond to The Epoch Times’ request for comment.
The influence that social media has on young girls is especially concerning to Aaliyah Kissick, a 24-year-old graduate student who has worked as a teen mentor.
“It’s amazing how persuasive these posts can be,” she told The Epoch Times. “It’s even more dangerous for people whose brains are developing because it’s targeting them based on commentary.”
Algorithms reach beyond the content a user is already engaging with, showing teens the kinds of videos their friends are viewing. Teens can be bombarded with content about the antidepressant Zoloft simply because that is what their peers are into, Kissick said.
“Unfortunately, when you get a bunch of people together talking about mental illness and ruminating on the symptoms rather than working toward solutions, it can create an echo chamber where you’re all just getting sicker,” she said.
Overreliance on Medication
Many current treatment approaches overlook the complex underlying factors contributing to teen anxiety, such as academic stress, social dynamics, family instability, and undiagnosed learning challenges, Dr. Cammy Benton, family physician and integrative practitioner, told The Epoch Times. These root causes often require a more holistic and developmental approach rather than immediate pharmacological intervention.
The increasing tendency to prescribe medication can inadvertently mask fundamental issues, potentially preventing teens from developing critical coping mechanisms and understanding the contextual origins of their mental health challenges.
In 2020, nearly 12 percent of children were told by a health care professional that they had depression or anxiety—up from 9.4 percent four years earlier.
Youth complaints of anxiety during doctor visits were three times higher in 2018 than in 2006, rising to 4.2 percent from 1.4 percent, according to a study in Pediatrics that examined data from the National Ambulatory Medical Care Survey of doctor visits among youth.
In that same period, anxiety diagnoses were three times as high in teens and nearly three times as high in young adults. The rate of those receiving therapy dropped to 33 percent from 49 percent.
About 62 percent of those diagnosed were given an anxiety medication, with 45 percent receiving SSRIs and 18 percent receiving benzodiazepines, which can be dangerous. Moreover, child psychiatrists were more likely to practice in high-income counties, counties with higher levels of education, and metropolitan counties versus surrounding areas. In other words, disparities limited access to these services.
SSRIs—particularly Prozac, Lexapro, Celexa, and Zoloft—are a first-line treatment for anxiety, along with cognitive behavioral therapy, which is psychotherapy that focuses on helping teens identify unhelpful patterns of thought and behavior and develop better coping strategies.

Prozac is often used as a primary treatment option for anxiety alongside cognitive behavioral therapy. (callumrc/Shutterstock)
“The reduction in therapy during office visits and the greater reliance on medications for anxiety disorders may reflect growing resource constraints in office settings in the context of a child and youth mental health crisis that has been building over time,” the authors of the Pediatrics study wrote.
That could be at least in part because of a geographical shortage of child psychiatrists. A Pediatrics report noted that while the profession was growing, access was not. In 2007 and 2016, 70 percent of U.S. counties had no child psychiatrist.
Any prescribing doctor can give a teenager SSRIs or other anxiety medications, which are considered safe by the American Psychological Association. The American Psychological Association did not respond to The Epoch Times’ request for input.
Doctors may not share adverse effects because they think that they are rare, Witt-Doerring said. Health care professionals may not discuss therapy or exercise, adequate sleep, and good nutrition—foundational factors that can contribute to poor mental health.
“Lifestyle changes can offer significant therapeutic advantages for patients, therapists, and societies, yet are insufficiently appreciated, taught or utilized,” psychiatry professor Dr. Roger Walsh wrote in an American Psychological Association article. Some of the lifestyle changes that he suggested include a healthy diet, time in nature, exercise, religious involvement, and recreation.
Witt-Doerring said medication should be a last resort, particularly for teens, and used only for immense suffering. A rush to a fast solution with drugs can turn into a game of Russian roulette, he said.
“If the system sees people in very transactional 15-minute visits where they just talk about drugs and don’t really try to help the person with the issues causing the problem, then that’s a big problem,” he said. “The fallout is there’s going to be a lot of people on these medications that can’t come off.”
Teen Anxiety Treatment and the Compliance Gap
Complicating teen anxiety and depression is the fact that teens are not stellar at
adherence—with medication or behavioral changes. Issues such as emotional maturity and developmental and family support systems influence their commitment to treatment.
Habit formation can be difficult at any age, Benton said.
In cases of complicated compliance, she said she likes to use magnetic resonance therapy, a form of transcranial magnetic stimulation that has shown promise for anxiety. Treatment sessions involve directing magnetic pulses to specific areas of the brain.
“It doesn’t require them to be compliant to things, because that’s super hard for them and then they feel like failures because they aren’t able to do what you tell them to,” Benton said.
Antidepressant Side Effects
Most antidepressant drugs work by numbing the brain in much the same way that alcohol and narcotics do. This can be therapeutic in severe cases of anxiety, Witt-Doerring said. However, relying on drugs also inhibits long-term resilience.
“The other thing that happens is some people end up feeling really flat on the medications, and so they become kind of somewhat dissociated from life,“ he said. ”They have less connection with people around them.”
Other consequences of taking SSRIs can be life-altering. Among them are:
- Suicidal thoughts and behaviors
- Mania
- Seizures
- Sexual dysfunction, including decreased libido, erectile dysfunction in men, and delayed or absent orgasm in women
- Discontinuation syndrome, which causes nausea, sweating, mood and cognitive issues, insomnia, and other symptoms after abruptly stopping medication
Some patients can experience these symptoms long after stopping drugs, Witt-Doerring said.
“Most young people put on antidepressants aren’t told they can cause permanent sexual dysfunction,” he said. “Some people—they never recover. That’s obviously a nightmare if that happens to you.”
Many are not warned about how difficult it may be to stop using SSRIs and other drugs. Protracted antidepressant withdrawal can affect one in six to seven patients who discontinue their medication.
Worse Off After Medication
A
survey of 1,148 mostly white female patients who wanted to quit taking antidepressant drugs found that 40 percent had withdrawal symptoms that lasted more than two years, and that 80 percent were moderately or severely affected by these withdrawal symptoms. Results published in the Journal of Affective Disorders Reports noted that 25 percent were unable to stop using their medication.
Problems with cessation could be because of protracted antidepressant withdrawal damaging the brain. More than 75 percent of survey respondents experienced new symptoms that are not common in anxiety and depression, including:
- Dizziness
- Memory problems
- Difficulty concentrating
- Increased sensitivity to light and noise
- Headaches
- Feelings of electric shocks in the brain
- Feelings detached or disconnected from the body or mind
- Feelings of detachment from surroundings, making the world feel distorted
Adverse effects of withdrawal included impaired work function (56 percent), loss of jobs (20 percent), need for sick leave (27 percent), and relationship breakdown (25 percent).
One qualitative study based on 69 patient narratives described two cases of suicide related to withdrawal symptoms, including one person with three years of unresolved sexual dysfunction who posted online on the day before taking her life that she did not think that she could go on in her current state.
According to the study, the 21-year-old patient said: “To be honest, now I’m in absolute hell. I don’t see much hope in this situation anymore. It’s been 3+ years, and I’m still in pretty much the same situation. I don’t know how much longer I’ll be here, honestly.”
On the next day, the young woman killed herself.
Another risk is tardive dysphoria, a condition of worsening depression after long-term antidepressant use.
“Sometimes getting on these medications just makes people worse over time,“ Witt-Doerring said. ”The doctors miss that the drug is making them worse, and then they just end up piling [other] drugs on them.
“Patients start accumulating multiple different drugs, and they’re still not getting better, but it’s actually the original drug that they were put on that’s harming them.”
Drug Snowball Effect
Crystal Weichelt’s long struggle with antidepressants began when she took an SSRI as a teen after a boyfriend breakup left her feeling anxious.
She told The Epoch Times that her anxiety increased, so her psychiatrist prescribed her a small dose of Ativan, a benzodiazepine used for anxiety. Benzodiazepines slow down the brain and nervous system and can become habit-forming. Overdose can result in respiratory depression and death.
“A person with anxiety is very vulnerable to begin with,“ she said. ”You will do anything that the doctor says to make these symptoms go away. That pill looks like the perfect fit for your life, and you’ve got this doctor saying this pill will help you.”
After 12 years on Ativan with a dose that gradually became 10 times stronger, Weichelt began to question why she continued to struggle with anxiety.
A Facebook benzodiazepines support group encouraged Weichelt to slowly taper off her medication. The process took 3 1/2 years, and she became increasingly sick even after she stopped taking them.
She ended up being bedbound for four years and homebound for five years. Her husband had to help her eat and shower. She weighed 100 pounds and was so sick that she had her funeral planned. Still, she did not give up hope.
“I have a very deep faith in God, and I knew he was going to carry me out of the storm, and he did,” Weichelt said. “I told God if I got through this to the other side, that I would help other people do the same.”
It has been more than two years since she has taken medication, and she has become a certified life coach to support others who are tapering off benzodiazepines.
Some of the techniques that Weichelt uses to help in recovery are:
- Mind–body visualizations
- Healing Scriptures and meditation
- Exercise, often starting with small movements from bed
- Community Zoom meetings so people know that they are not alone
Drug Abuses and Misuses
“Adolescence is a vulnerable period for risks from medications that carry a potential for misuse and abuse,“ Greta Bushnell, assistant professor of epidemiology at Rutgers School of Public Health, told The Epoch Times in an email. ”This age range is characterized by a heightened risk of drug misuse, increased risk-taking behavior, initial exposure to illicit substances, and is also when many symptoms of mental health conditions present.”
Bushnell noted that non-pharmacological treatment options should be considered for struggling teens, in addition to the safest medication options.
Cautious prescribing of sedative, hypnotic, and anti-anxiety drugs—benzodiazepines and others—in younger people is vital, she said.
Bushnell was lead author of a study recently published in Addiction showing that disorders related to recurrent use of sedative, hypnotic, and anti-anxiety medications have increased fivefold in teens and young adults since 2001. Nevertheless, such abuses remain relatively uncommon.
The increase in these disorders, which include withdrawal, intoxication, and addiction, remains low and could be driven by an increase in detection and awareness, according to Bushnell.
“Medications used to treat anxiety disorders vary in their effectiveness and safety profile,“ she said. ”Therefore, treatment choice depends on a variety of factors. Benzodiazepines, for example, come with concerns related to misuse, abuse, and overdose and are not recommended in certain patients.”
Benzodiazepines are considered a second-line treatment strategy for depression and anxiety, and taking them—either alone or along with SSRIs—increases the likelihood of overdose compared with SSRI use alone, according to 2023 research published in Addiction.
The medications are also used for issues beyond depression and anxiety, such as sleep disorders and seizures. Most teens misusing the drugs in the Addiction study did not have a prescription but were accessing them through friends or medicine cabinets. Side effects of such misuse could be misinterpreted as an anxiety disorder.
Hope Beyond Drugs
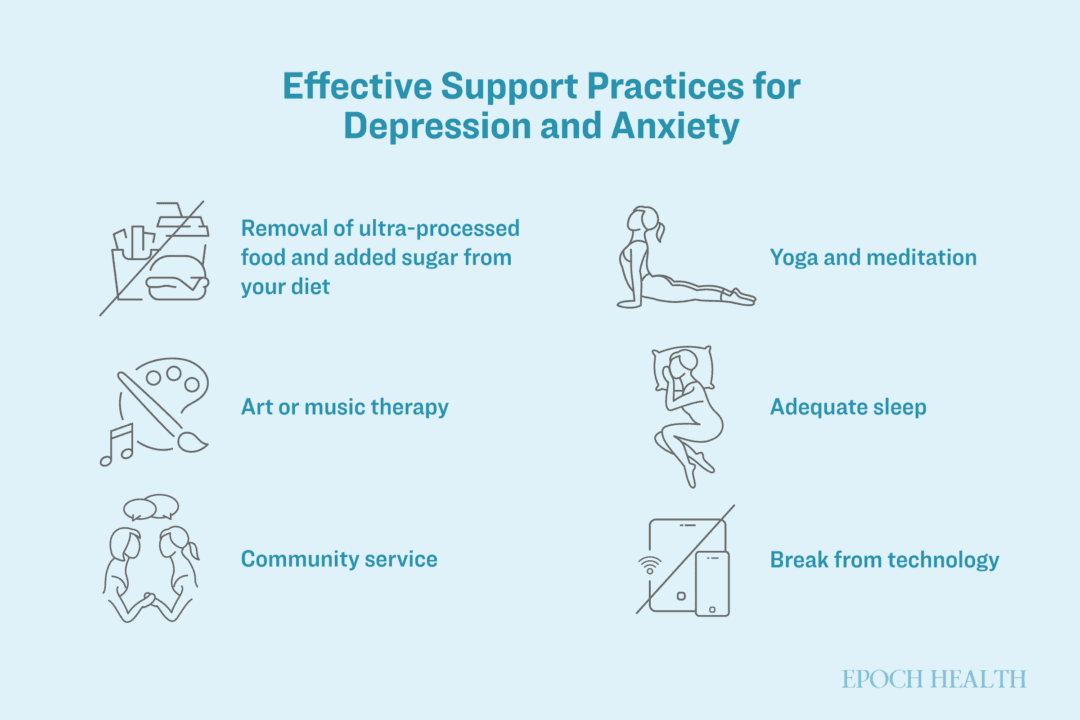
Besides medication and therapy, other supportive practices can be effective for symptoms of anxiety and depression.
Some of the most impressive research, Witt-Doerring said, is on nutrition. Teen mental health is improved when removing ultra-processed foods and sugar from the diet. Mediterranean and ketogenic diets have also been associated with improved brain function.
Many programs that specialize in teen anxiety offer a range of holistic activities and therapies, such as one at Newport Academy that treats teen mental health and substance use disorders. These programs emphasize many types of treatments, including physical activity, art or music therapy, community service, yoga and meditation, adequate sleep, and breaks from technology.
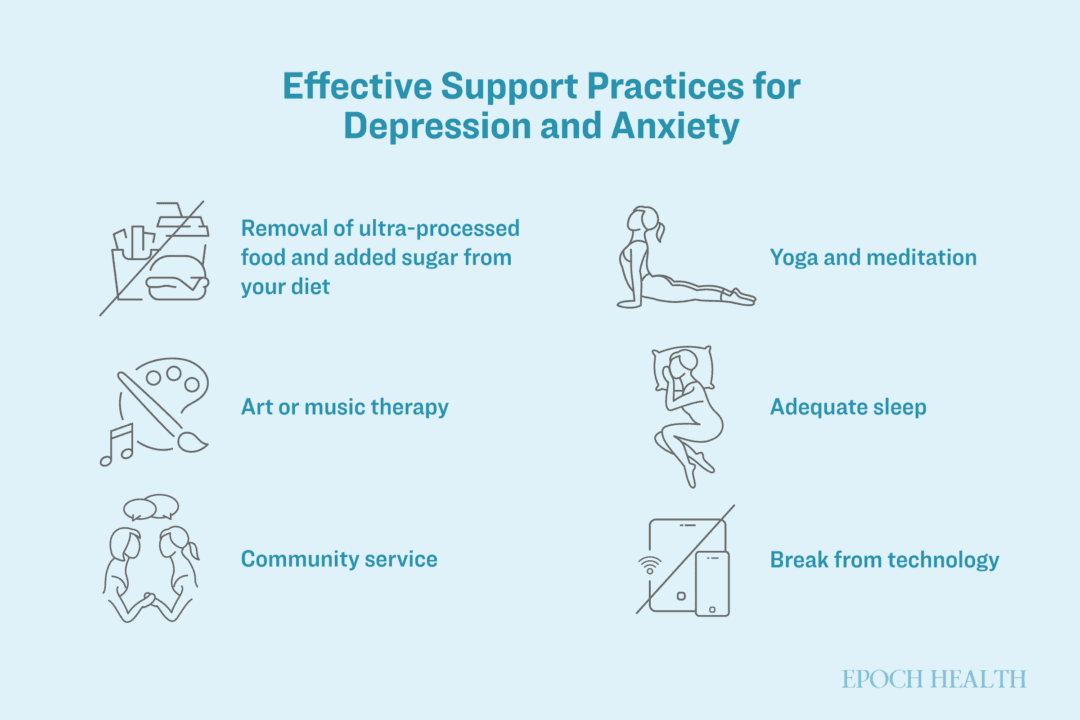
Illustration by The Epoch Times, Shutterstock
Research has shown that four months of exercise—such as brisk cardio for 30 minutes three times per week—is as effective as SSRI treatment with Zoloft.
Establishing healthy phone habits helped Kissick. She said she takes breaks from social media frequently. Her Christian faith and friendships also help alleviate anxiety by reinforcing her identity and purpose.
“A big part of physiological safety is having friends, having a community, and having something bigger than yourself to believe in,” she said. “I think forming in-person communities is going to be the antidote to this.”
Courageous Metamorphosis
The transition from teen to adult also requires a bit of patience, as Sofia noted. Just as her appearance is rapidly changing, her inner character is being molded—a process that Sofia described as influenced by hard choices.
Sofia said that while she values eating healthy and exercising, there are times she hates doing both. Growth has meant pushing through a lack of desire.
“Nothing changes unless you change it, and some people either crash or fly with that mentality,” she said.
Sofia rejected medicine and decided to boost her self-confidence with a discipline of meditation, positive affirmations, and facing her fears, even if that meant being red-faced and sweaty in social situations.
A big part of Sofia’s journey is her inner narrative—telling herself that she wants to wake up early, that she does not want to use her phone before bed, and that she will be courageous and talk to people. She found that shifting her perspective and perceiving herself as someone who is confident and sociable revealed to her that she actually enjoys being around a variety of people, even those different from her.
“I don’t think the answer to it all is pills and seclusion,“ Sofia said. ”I think ... doing stuff that’s good for your soul—like going on hikes, getting nine hours of sleep, eating things that are good for you, treating your mind and body as a temple—all of those things grew me into who I am now.”
If you (or a loved one) are struggling with thoughts of suicide or self-harm, it is important to reach out for support. Please remember, you are not alone.
National Suicide Prevention Lifeline: Call or text 988 or text “HELLO” to 741741