Advisers to the Centers for Disease Control and Prevention on April 16 recommended that the agency expand the availability of vaccines against the respiratory syncytial virus, or RSV.
Adults with at least one risk factor for RSV should be able to receive a vaccine, the Advisory Committee on Immunization Practices said in a 14–0 vote, with one member abstaining.
“What’s swaying me is there clearly are people in that 50 to 59 year sort of age group—for example lung transplant patients, hematopoietic stem cell transplant patients—that would clearly benefit from having access to this vaccine,” Dr. Jane Zucker, one of the members who voted in favor of expanding access, said after the panel was presented with data on the RSV vaccines during a meeting.
Dr. Jason Goldman, a liaison to the panel for the American College of Physicians, told members he has patients who are 50 and older with risk factors who have told him they want the vaccine, but have not been able to get it.
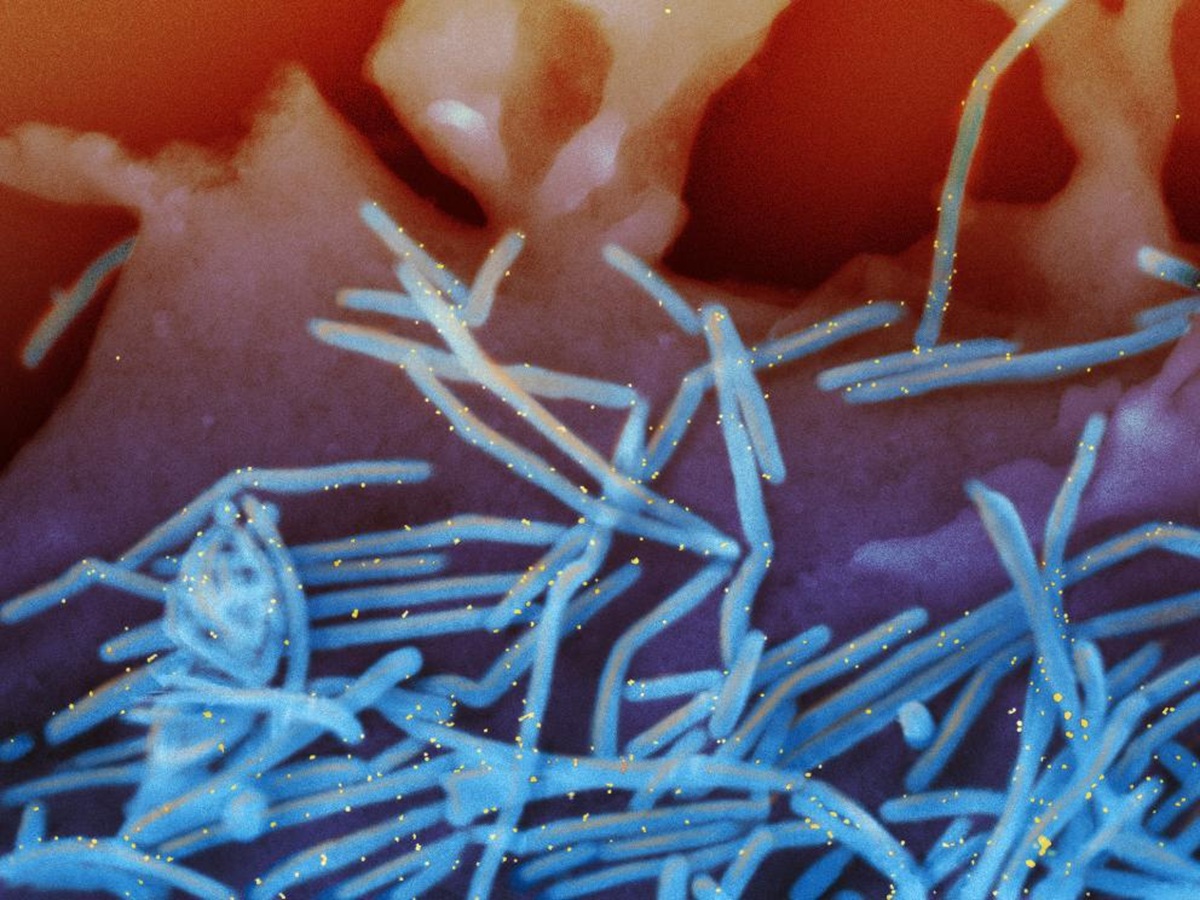
RSV is a virus that primarily causes a cold and other mild symptoms, but can lead to hospitalizations and even deaths, particularly in older individuals. According to the CDC, RSV leads to more than 100,000 hospitalizations among adults aged 60 and older each year.
Three RSV vaccines, from GlaxoSmithKline, Pfizer, and Moderna, are currently licensed in the United States. The GlaxoSmithKline and Pfizer shots, both protein subunit vaccines, are licensed for people younger than 60, but access requires CDC signoff.
The CDC typically accepts recommendations from its vaccine advisory panel, but not always. The agency has not yet issued a comment on the RSV vaccine recommendation.
In 2024, the CDC recommended that all adults aged 75 or older, and adults aged 60 to 74 who have a higher risk of contracting RSV, receive an RSV vaccine, following advice from the advisory panel.
A subgroup of experts on the panel who studied the matter in-depth split over whether to provide access to the RSV vaccines to the 50–59 age group, according to a presentation. A majority said that there were moderate desirable anticipated effects of expanding access, such as preventing some hospitalizations, and a small amount of undesirable expected effects, such as Guillain-Barre syndrome, which authorities say has been linked to the shots. A minority said that the risk-benefit calculus may not favor intervention, and there was not sufficient information at present to decide.
None of the advisers in the minority ended up outlining the issues during the meeting. Dr. Michael Melgar, a CDC employee who assisted with the analysis, said the split stemmed from uncertainty.
“I think some work group members are concerned about the uncertainty in the magnitude of risk of Guillain-Barre Syndrome,” he said.
Several people speaking during the public comment period offered support for expanding RSV vaccine access, including Sam Sears, a health policy associate with the National Consumers League.
A meeting later this year will go over whether to recommend the CDC let people younger than 50 receive an RSV vaccine, the CDC said.
Wednesday’s meeting was the first time the panel had met since Health Secretary Robert F. Kennedy was sworn in as head of the Department of Health and Human Services, which is the CDC’s parent agency.
The panel had been set to convene in February. The meeting was delayed to give the public more time to provide feedback on agenda items, a health official said previously.
Advisers also voted to advise the CDC to expand access to chikungunya vaccines, which were also recommended for the first time in 2024, and meningococcal vaccines. The votes were also unanimous, apart from one abstention in the vote for chikungunya vaccines.