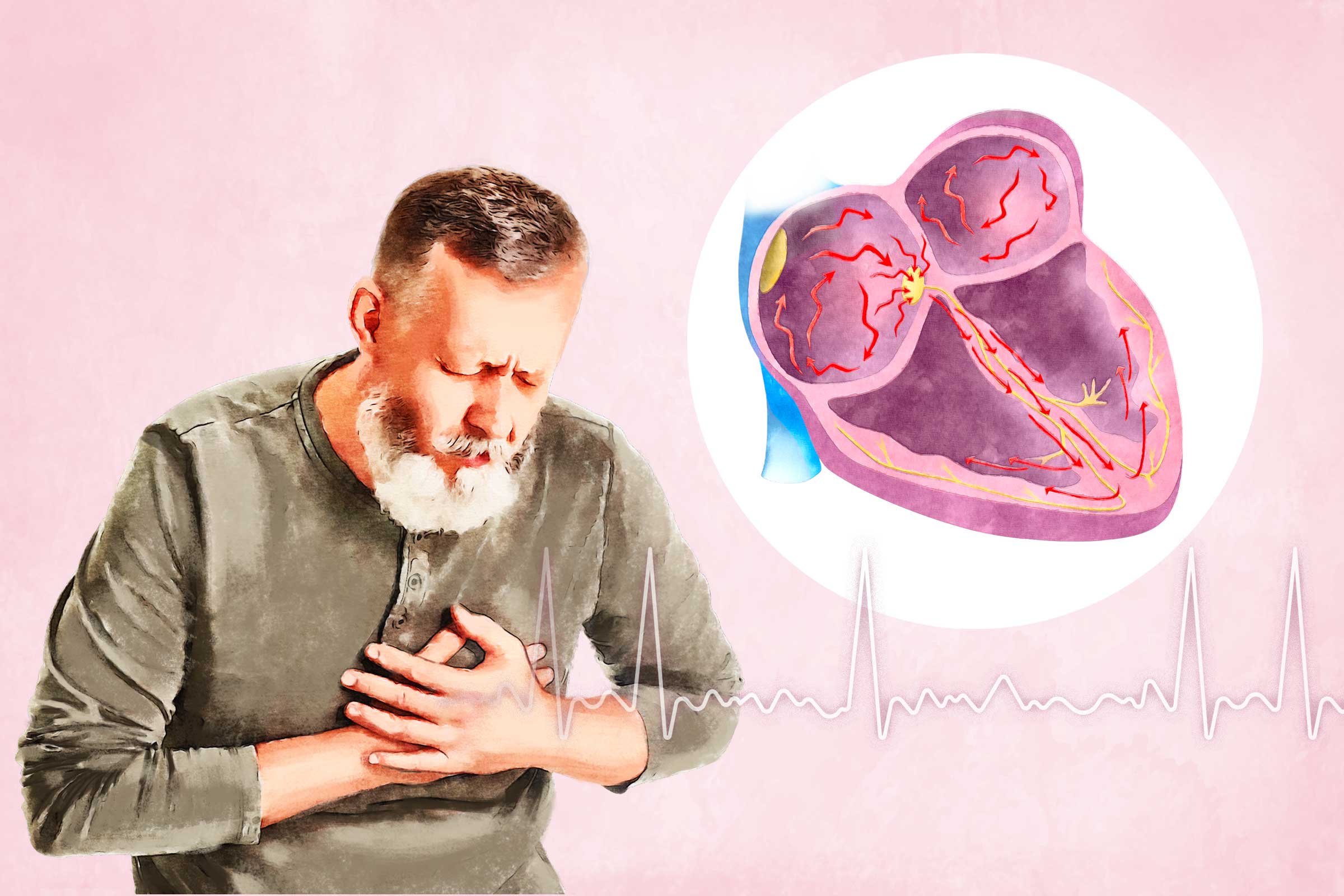
A-fib symptoms vary from person to person. Common symptoms include:
- Heart palpitations (rapid, fluttering, or pounding heartbeat)
- Low energy or fatigue
- Shortness of breath
- Trouble exercising or performing everyday activities
- Lightheadedness or dizziness
- Fainting
- Low blood pressure
- Fluid buildup in the legs, ankles, or feet
- Blood clots
- Chest discomfort, pain, or tightness
Some people recognize the occurrence of A-fib by experiencing noticeable heart palpitations, while others have no symptoms and only learn of the condition through a physical examination.
Medical Conditions
- Congenital heart defect: Structural abnormalities that affect the heart’s electrical system
- Heart valve disease: Leaking (regurgitation) or stenotic (narrowed) heart valves that enlarge heart chambers and interfere with electrical impulses
- Coronary artery disease: Restricted blood supply to the heart, leading to tissue damage and electrical instability
- Sleep apnea: Disrupted breathing patterns during sleep that strain the heart muscle and affect electrical pathways
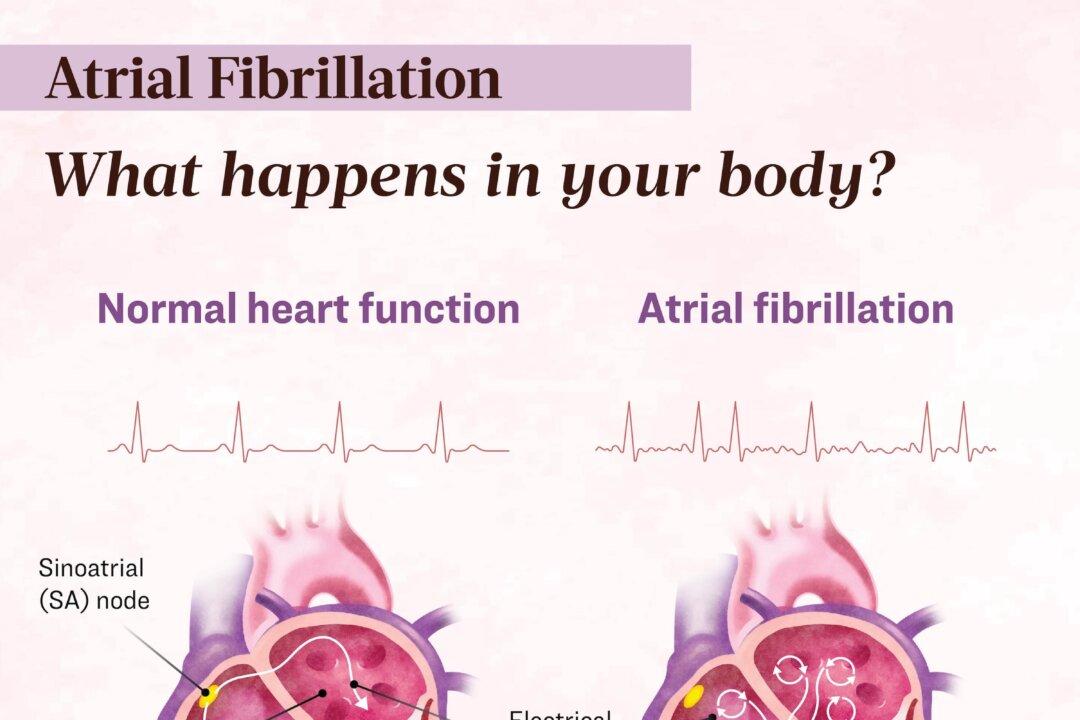
- Sinus node dysfunction: Malfunctioning of the sinus node, a natural pacemaker, that causes the heart’s upper chamber or atria to twitch rather than contract normally
Health Problems
- Heart attack
- High blood pressure
- Overactive thyroid (hyperthyroidism)
- Lung infections, such as pneumonia
- Viral infections
Lifestyle Factors
- Using illegal drugs
- Drinking excessive alcohol or caffeine
- Smoking
- Taking stimulant-containing cold and allergy medications
Paroxysmal A-fib
Also known as intermittent A-fib, paroxysmal atrial fibrillation (PAF) occurs when an irregular rhythm resolves within seven days of onset. According to a 2001 study published in the National Library of Medicine, PAF is estimated to account for anywhere from 25 percent to 62 percent of A-fib cases.
Persistent A-fib
When A-fib lasts more than seven days, it is classified as persistent and is the most common type of A-fib.
Long-Standing Persistent A-fib
A-fib lasting longer than 12 months is classified as long-standing persistent.
Permanent A-fib
When A-fib persists despite medication or surgical intervention, it is classified as permanent.
- Stage 1: At Risk for A-fib Risk factors such as lifestyle, weight, and diabetes may be controllable, while others, such as age or genetics, are not.
- Stage 2: Pre-A-fib The heart shows early signs of electrical changes that could lead to A-fib. Treatment and closer monitoring begin to prevent progression.
- Stage 3: Diagnosed A-fib A formal diagnosis is made. Treatment focuses on controlling heart rate and rhythm with medications, procedures, or both. Stroke risk increases, so blood thinners may be recommended.
- Stage 4: Permanent A-fib A-fib persists despite treatment. Management focuses on symptom control and regular stroke risk assessment.
- Age: A-fib becomes more common with age, affecting about 70 percent of people with irregular heart rhythms between 65 and 85.
- Family history: Certain genetic mutations can increase the likelihood of developing A-fib.
- Medical conditions: Heart, lung, and sleep disorders can contribute to irregular heart rhythms.
- Race: A-fib is more common in white people of European descent.
- Stress or panic disorders: Chronic stress or anxiety can trigger irregular heartbeats.
- Unhealthy habits: Smoking, excessive alcohol consumption, and illegal drug use can strain the heart and increase A-fib risk.
- Obesity: Excess weight puts added stress on the heart and may contribute to electrical disturbances.
- Surgical procedures: Surgeries involving the heart, lungs, or esophagus can affect heart rhythm.
- Chronic kidney disease: Reduced kidney function is linked to a higher risk of A-fib.
- Heart valve disease: Leaking or narrowed heart valves can lead to irregular heart rhythms.
- High blood pressure: Increased pressure forces the heart to work harder, which can contribute to A-fib.
- Diabetes: High blood sugar levels can damage blood vessels and increase A-fib risk.
- Hyperthyroidism: An overactive thyroid can overstimulate the heart, leading to irregular rhythms.
- Sleep apnea: Interrupted breathing during sleep can strain the heart and affect its electrical system.
- Chronic obstructive pulmonary disease (COPD): Lung disease can lead to reduced oxygen levels and increased heart strain.
Basic Diagnostic Tests
- Electrocardiogram (EKG): Records the heart’s electrical activity and can detect A-fib if it occurs during the test
- Holter monitor: A portable EKG worn for days or weeks to catch irregular heart rhythms that occur intermittently.
- Loop recorder: A small implanted device that continuously tracks heart rhythm over months or years
Imaging Tests:
- Echocardiogram: An ultrasound of the heart that evaluates chamber size, pumping function, and possible blood clots
- Chest X-ray: Helps detect an enlarged heart or fluid buildup in the lungs
- Cardiac magnetic resonance imaging: Produces detailed images of the heart’s structure and function to assess abnormalities
Other Assessments:
- Blood tests: Measures thyroid function and checks for other conditions that may contribute to A-fib
- Sleep study: Identifies sleep apnea, a common trigger for A-fib
- Exercise stress test: Evaluates how the heart responds to physical activity and detects abnormalities that may not appear at rest
Stroke
The erratic electrical signal in A-fib causes the heart’s upper chambers to quiver instead of contracting properly. This prevents blood from moving forward efficiently, causing it to pool inside the heart. When blood is not moving freely, it can form clots. If a clot travels through the bloodstream and blocks a small artery in the brain, it can cause a stroke.
Heart Failure
Heart failure occurs when the heart weakens and cannot pump enough blood to meet the body’s needs. In A-fib, the heart beats so quickly and irregularly that it can’t fill appropriately between beats, reducing the amount of blood pumped with each contraction. This can lead to blood backing up into the lungs, causing shortness of breath, swelling in the feet and ankles, and fluid-related weight gain.
Dementia
A 2018 study published in the Journal of the American Heart Association found that A-fib was linked to an increased risk of dementia and cognitive decline. A-fib can also cause recurrent silent strokes—small, undetected strokes that don’t have overt symptoms but contribute to gradual brain function deterioration.
- Control heart rate and rhythm
- Prevent blood clots and reduce stroke risk
- Restore the heart to a normal rhythm
- Address underlying conditions and complications
- Reduce risk factors that can worsen A-fib
Medications
Medications are an essential part of A-fib treatment and may need to be taken for life.
- Rate control medications: Slow the heart rate and prevent the heart muscle from weakening. Examples include: beta-blockers such as metoprolol and atenolol
- Rhythm control medications: Also called anti-arrhythmic drugs, these help maintain a regular heart rhythm
- Blood thinners: Also called anticoagulants, help prevent blood clots and reduce the risk of stroke
More Invasive Procedures
If medications do not effectively control A-fib, procedures may be necessary to restore a normal heart rate and rhythm.
- Electrical cardioversion: A procedure that involves using a controlled electrical shock through a defibrillator to reset the heart’s rhythm. If A-fib is severe, cardioversion may be performed immediately. Otherwise, doctors usually wait three to four weeks after starting blood thinners to reduce the risk of stroke from potential clots. Blood thinners are continued for at least four weeks after the procedure.
- Catheter ablation: A minimally invasive procedure in which a doctor inserts a thin, flexible tube (catheter) into a blood vessel in the groin and guides it into the heart. Heat or cold energy is used to create small scars in the heart tissue, disrupt the irregular electrical pathways in the heart, and help restore a normal rhythm. Catheter ablation can sometimes cure A-fib altogether.
- Maze Procedure: Performed during open-heart surgery, this procedure involves creating scar tissue in the heart using a scalpel. The scars disrupt abnormal electrical signals. Many people planning a coronary bypass or heart valve surgery also receive a Maze procedure.
- Left atrial appendage closure: A procedure that seals off a small sac in the heart’s upper left chamber where blood clots often form. A closure device is advanced through a catheter to the left atrial appendage, where it remains permanently.
Alternative Therapies
- Yoga therapy: This has been shown to promote general health and well-being and positively affect many chronic medical conditions. Yoga can also play a key role in treating A-fib due to its impact on the autonomic nervous system. Studies suggest that yoga may help lower resting heart rate, reduce A-fib triggers, and decrease stress and oxidative damage that contribute to heart muscle changes.
- Acupuncture: Although studies are limited, one trial assessed how effective acupuncture was for restoring normal heart rhythm (cardioversion) in A-fib patients. Researchers found that 85 percent of patients achieved cardioversion with acupuncture compared to 67.5 percent of those treated with the anti-arrhythmic drug amiodarone. A 2017 review of 13 randomized controlled trials suggested that acupuncture can help restore normal heart rhythm and improve recovery time.
- Biofeedback: This therapy uses a monitor to show heart rate or breathing patterns. Patients practice relaxation techniques like deep breathing to help slow their heart rate. Although a small study in 1973 showed potential benefits for A-fib, biofeedback is not yet widely used for this condition.
Herbal Medicines
Shensongyangxin is a Chinese medication approved for treating arrhythmias. Interestingly, the same Journal of Thoracic Disease study found that Shensongyangxin was as effective as the anti-arrhythmic medication propafenone in treating paroxysmal A-fib. However, because of the limited evidence, Shensongyandxin should be used with caution.
Health Factors
- Cholesterol levels: Keeping cholesterol within a healthy range reduces heart strain.
- Blood pressure: Managing blood pressure helps prevent heart damage.
- Blood glucose: Controlling blood sugar levels lowers the risk of heart-related complications.
Behavioral Factors
- Smoking: Avoiding cigarettes reduces inflammation and heart strain.
- Physical activity: Regular exercise strengthens the heart and improves circulation.
- Diet: A heart-healthy diet supports overall cardiovascular function.
- Body mass index: Maintaining a healthy weight helps reduce heart disease risk.
Simple Steps to Help Prevent Atrial Fibrillation
In addition to managing Life’s Simple 7 risk factors, making small but meaningful lifestyle changes can further reduce the likelihood of developing A-fib. These steps include:
- Exercise for at least 30 minutes per day, or as tolerated
- Limit alcohol intake
- Stop smoking
- Eat a heart-healthy diet
- Maintain a healthy weight
- Treat underlying conditions such as hypertension, heart valve disease, and atherosclerosis
Adopting a healthier lifestyle and recognizing and avoiding common triggers can reduce the incidence of A-fib or possibly prevent it altogether.