Proper nutrition and physical activity are widely accepted tools in preventing chronic disease. However, some doctors have begun to embrace another tool: vagus nerve stimulation.
Navaz Habib, a chiropractor certified in functional medicine, stresses the importance of diet and exercise, but the vagus nerve also plays a big role in his wellness strategy. He’s written two books on the subject, the most recent titled “Upgrade Your Vagus Nerve.” The book explores the research, methods, and benefits of stimulating the vagus nerve, such as inflammation control, better immunity, and more.
“I’ve seen improvements in my clients from depression to concussion recovery to Parkinson’s symptoms to digestive discomfort and IBS,” Habib said.
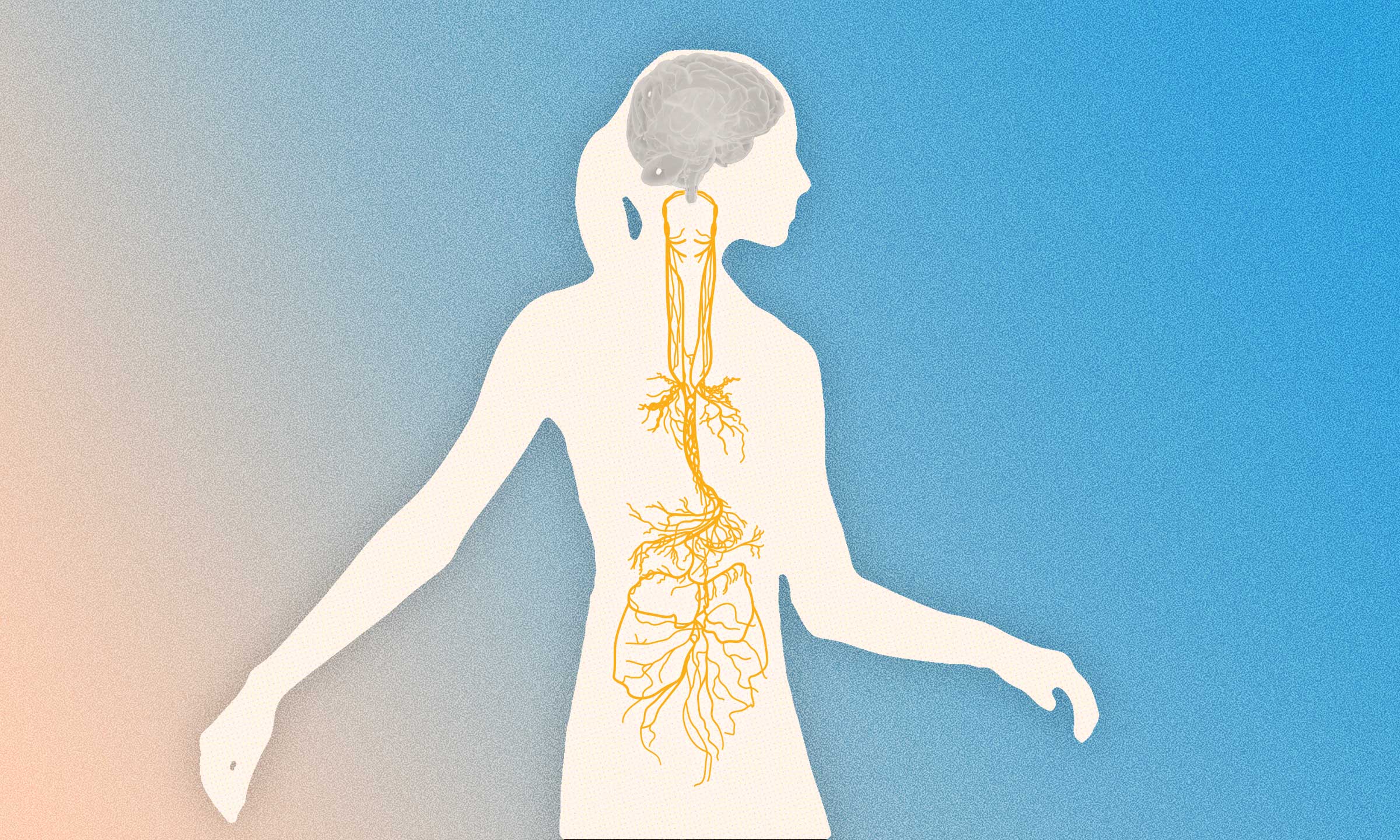
Understanding the Vagus Nerve
For centuries, doctors have understood the vagus nerve to be a major nerve network in the body. The longest of the body’s 12 cranial nerves, the vagus nerve connects the brain to the abdomen and virtually everything in between.
“It’s a very unique nerve,” Habib said. “It is the only cranial nerve that leaves the head cavity and the only nerve in the body that connects to essentially every visceral organ.”
The name “vagus” comes from a Latin word that means wandering. When it’s working properly, the vagus nerve network presides over a diverse array of functions—influencing the immune, cardiovascular, digestive, respiratory, and endocrine systems.
Vagus nerve stimulation as a recognized form of treatment goes back to the 1880s when New York neurologist James Corning developed a device to send an electric current through the nerve as a way to treat epilepsy. It didn’t take off back then, but the idea was rediscovered about a century later when an implantable device was approved by the U.S. Food and Drug Administration (FDA) in 1997 to prevent seizures.
Modern Applications
Since then, a significant body of research has examined vagus nerve stimulation as a way to treat a variety of
health conditions, including diabetes, obesity, Alzheimer’s disease, headache, cardiovascular disease, arthritis, sleep problems, depression, and more.
Most recently, vagus nerve stimulation has shown promise as a treatment for long COVID, a condition that some believe may, at its core, be related to nerve inflammation.
The Centers for Disease Control and Prevention says that those with long COVID can have a “wide variety of symptoms that can range from mild to severe and may be similar to symptoms from other illnesses.” Symptoms can include dizziness, gastrointestinal disorders, a racing heartbeat, cognitive problems, and shortness of breath.
While these symptoms may seem unrelated from a distance, they can all be traced to a vagus nerve in distress. That’s because the vagus nerve covers a lot of ground.
The Functionality of the Vagus Nerve
The vagus nerve is perhaps best known for managing the body’s
parasympathetic nervous system, otherwise known as our relaxation response. Habib explains that vagus nerve stimulation doesn’t cure any particular condition, rather it enables the body to better heal itself.
“Our bodies cannot heal when we’re in a sympathetic fight or flight state. They need to enter that parasympathetic, rest, digest, and recovery state, and that’s where the healing process can occur,” he said.
Another key aspect of healthy vagus nerve tone in mitigating chronic disease is that it keeps inflammation in check.
“We know that in most chronic health conditions, uncontrolled inflammation is the common path to disease. So what it comes down to is that we can control that inflammatory function,” Habib said.
Stimulating the Vagus Nerve: Options and Techniques
You don’t need to get an implant to stimulate your vagus nerve. In fact, people have been self-stimulating it for millennia, though they may not have known about the vagus nerve at all. Habib teaches several technology-free techniques that anyone can perform, such as breathing exercises, chanting, humming, and singing.
While significant scientific details regarding the vagus nerve have emerged in recent years, the fundamental understanding of its functions has been available for centuries, particularly in the realm of deep breathing techniques such as pranic breathing found in yogic practices, according to J.P. Errico, a neuroimmunology expert.
“Holding your breath and exhaling in a controlled manner stimulates the vagus nerve,” Errico told The Epoch Times.
Deep breathing activates special nerves in the lungs, known as pulmonary stretch receptors, which in turn activate the vagus nerve, stimulating the parasympathetic nervous system, which is responsible for regulating the body’s rest-and-digest response.
“When you’re only shallow breathing, because you’re stressed or in fight-or-flight mode, you’re not stimulating it, because you’re not getting that signal through those stretch receptors,” Errico added.
In addition to deep breathing, other self-initiated techniques for stimulating the vagus nerve include humming, gargling, chanting, and singing.
These methods promote stimulation through vibration rather than stretch receptors. Since the voice box is located near a branch of the vagus nerve that runs through the neck, these vocalizations can gradually induce a sense of peace and calm.
Another stimulating method involves exposure to cold. A 2018 study found that applying cold stimuli, especially to the neck, can enhance cardiac-vagal activation.
However, these self-stimulating techniques work much more slowly than electrical stimulation. This is by design, Errico noted.
“Think about it,” he said. “Fight or flight is a survival state. It shouldn’t be easy to get out of that state. You shouldn’t be in the middle of fighting for your life and then suddenly calm.”
Emerging Technologies for Vagus Nerve Stimulation
However, Habib says electrical stimulation is a more direct and efficient method.
“What I’ve found is when we use electrical stimulation, we get results far more quickly,” he said. “We’re able to accelerate the process of healing within the vagus nerve itself.”
For the implant, the stimulator is physically wrapped around a vagus nerve bundle and connected to a pulse generator placed in the chest, similar to a pacemaker. These units cost tens of thousands of dollars and the price of implantation. However, the benefit this unit can deliver, particularly for drug-resistant epilepsy “can equal or exceed the purchase price of the device,” according to one comparative study.
In addition to epilepsy, this implanted device is also approved to treat depression. However, as doctors and researchers grasp the potential to treat a wider number of conditions with stimulation, interest has grown for a less expensive, noninvasive stimulator.
One option that has emerged is a wearable device with electrodes placed near the ear canal. A large clinical study sponsored by the Massachusetts General Hospital is currently evaluating this strategy in treating gastrointestinal issues.
But Habib prefers another option. The device he uses on his patients and himself is a small handheld unit that runs between $300 and $500.
This device, known as Truvaga, was developed by Errico, who has been in the medical device-making business since the 1990s and has more than 250 patents to his name. Errico said he had been mulling over the idea of a nerve-stimulating device for years following a brief but enlightening discussion with a neurosurgeon.
“He was one of the very first people to start using deep brain stimulation to treat Parkinson’s and essential tremor. And I was absolutely flabbergasted when I saw the results of his surgeries,” Errico said. “By getting to the right location in the brain and stimulating it with the right parameters, he could stop a patient from shaking, and all the symptoms would go away with no side effects. That was pretty much as close to magic as I'd ever seen, and I knew that I wanted to get involved.”
Clinical research for Errico’s vagus nerve stimulator began in 2006, and initial studies showed that his design was effective, but he wanted to create something more accessible than an implant. “We actually did FDA-approved pilot studies that worked beautifully,” Errico said, “but what we realized was that it wasn’t very user friendly, and we needed to figure out a way to do it noninvasively.”
The result of his team’s effort led to a device known as gammaCore, a small handheld unit that is the only FDA-cleared noninvasive device to treat various kinds of headaches via the vagus nerve. Errico says the gammaCore device is still available by prescription, but Truvaga is the direct-to-consumer version.
Errico makes a third version for the military called TAC-STIM. The name refers to the tactical advantage that stimulation is said to offer. “For the last eight years, the military has been studying the use of vagus nerve stimulation, along with other types of neuromodulation, to see if it can actually make people smarter,” Errico said.
Research and Promising Outcomes
This research is a project under the Defense Advanced Research Projects Agency called the TNT (targeted neuroplasticity training) program. It investigates the use of noninvasive neurotechnology in combination with training to improve long-term retention of new cognitive skills.
One study published earlier this year in Nature shows that Errico’s device may offer just the kind of enhancement the military is looking for. Researchers showed that subjects who used the unit improved their ability to pick up and retain second-language vocabulary. Benefits were maintained across a 24-hour retention interval with no stimulation at the final test. The unit also helped subjects reduce fatigue and improve focus.
Subjects were “highly selected career linguists at the US Department of Defense’s premier language school.”
“These are people who are motivated, focused, good at what they do, and we were still able to demonstrate in every application anywhere from a 25 to 40 percent improvement,” Errico said.
Errico’s device not only outperformed the ear-stimulating device, but researchers wrote that his unit was “an effective learning acceleration tool that can be utilized at language-teaching and other institutions focused on intensive training of cognitive skills.”
The Science Behind Mental Acuity Enhancement
How can stimulating a nerve improve mental acuity? Errico said that when you stimulate the vagus nerve, it releases a chemical called
acetylcholine.
“That acetylcholine moves throughout the brain, and it quiets any of those immune cells that happen to be distracted by inflammation. It really helps you focus. It really gets your brain working optimally,” he said.
Errico details the science behind vagus nerve stimulation in his recent book “The Vagus-Immune Connection.”
While there are several reported benefits to vagus nerve stimulation, there is also a vulnerability to this nerve, as some people can inadvertently produce a negative reaction. Known as the vasovagal response—the condition can be brought on by pain or emotional upset, which can cause light-headedness, a sudden drop in blood pressure, and possibly fainting or syncope.
But Errico ensures that this reaction won’t happen with Truvaga.
“In the vagus nerve bundle, there are multiple different types of fibers that cause things like bradycardia, bronchoconstriction, and syncope [that] are called C fibers, and they have a threshold for being activated that is about 15 to 20 times higher than the A fibers [that the device targets],” he said. “So we are not stimulating those. In fact, our device is incapable of stimulating at that higher level.”
Safety and Usage Guidelines
Truvaga is designed to be safe and easy to use, but the manual cautions against those with a pacemaker or a hearing aid implant from using the product. The manual also warns against using it in a strong electromagnetic field or if you have an open wound, rash, or infection on your neck.
Elizabeth Tringali, a board-certified physician assistant who runs an integrative family practice in West Palm Beach, Florida, says she’s been using it on her patients for about two years with good results.
“It’s miraculous,” she said.
Tringali mentioned one patient—a 40-year-old woman who was having anxiety attacks. “She was flipping out,” Tringali said. “We called 911 just to make sure she wasn’t having a heart attack.”
Within minutes after using the Truvaga device, the patient calmed down. “She told the paramedics they didn’t need to stay. She was like a new person,” Tringali said.
Since vagus nerve stimulation can help activate the parasympathetic nervous system, Tringali says Truvaga can be very helpful for patients stuck in sympathetic dominance.
“We inherit these patients with all these chronic illnesses, and they just can’t get out of fight or flight from being sick for so many years,” she said. “They are on 20 medications and have tried everything under the sun.”
Tringali lets patients try the device in her office, and if they like it, they may purchase a unit to use at home. She says some results are immediate, while others take time to manifest.
“People will say, ‘You know what, I feel better.’ And if they stay on it, if I can get them to do it every day, you‘ll see their labs change. They’ll have more energy. And they respond to whatever treatment I’m doing,” Tringali said.
How to Use Truvaga
Truvaga is about the size of a deck of cards and includes two metal electrodes that users place on the left side of their throat.
“It’s where you would feel for your pulse,” Errico said. “You place the two electrodes in that notch, and then you begin to turn up the amplitude. The very first thing you'll feel is a little tingling at the skin.”
Errico says this particular place on the neck that the unit targets offers the best opportunity for stimulation. “That’s where the largest number of fibers are,” he said.
A bit of contact gel (such as the type used on an EKG machine) helps carry the current from the device to the skin. Users can control the amplitude of the device, typically setting it low when they first begin and turning it up once they get used to the feeling.
Errico says even dogs like it. “As soon as they see the device, they'll roll over and expose their neck,” he said. “It calms them down. They like it.”
The least expensive version of the device is called Truvaga 350. The drawback is that it has a limited number of uses (only 350 two-minute sessions or about six months’ worth of treatments if used twice daily). The pricier models have an unlimited number of uses but require an app installed on your phone.