A panel of experts selected by Health Secretary Robert F. Kennedy Jr. on Dec. 5 voted to recommend federal officials stop directing parents to get their infants quickly vaccinated against hepatitis B, unless the babies’ mothers test positive for the virus.
The Centers for Disease Control and Prevention currently recommends virtually all newborns receive a hepatitis B vaccine within 24 hours of birth. The CDC should, moving forward, no longer recommend that infants born to women who test negative for hepatitis B receive a vaccine against the virus, unless parents and health care providers decide to have the infants vaccinated following consideration of the risks and benefits of vaccination, according to a majority of the Advisory Committee on Immunization Practices (ACIP).
Members who voted in favor said safety and effectiveness data for the current recommendations are inadequate.
“What we are trying to do here is to go back to basic, good public health policy that is based on risk, that is based on informed consent and individual decision-making, when parents can think about the assessment of the risk and the benefits and make a decision,” Retsef Levi, one of the members, said ahead of the vote.
The CDC’s director typically adopts ACIP’s advice without alteration. Jim O'Neill, who is also Kennedy’s deputy secretary, is serving as acting CDC director.
The CDC’s parent agency, the Department of Health and Human Services, highlighted ACIP’s votes in a press release in which O'Neill was quoted as saying, “The American people have benefited from the committee’s well-informed, rigorous discussion about the appropriateness of a vaccination in the first few hours of life.”
The agency declined to say whether O'Neill would be accepting the advice.
Hepatitis B
Hepatitis B is a virus that causes problems such as dark urine and liver infection. It can be transmitted via exposure to bodily fluids from an infected person, as well as from a mother to child during pregnancy.
About 0.5 percent of pregnant women test positive for hepatitis B, and in 2021, 17,827 children were born to mothers who tested positive, according to an estimate from the National Center for Health Statistics. While about eight in 10 births overall that year were to U.S.-born mothers, a majority of mothers who tested positive for hepatitis B were not born in the United States.
Roughly 80 percent of children born in the United States in 2020 and 2021 received a hepatitis B vaccine dose within three days of birth, according to the CDC.
Officials have since 1991 recommended that all infants receive a hepatitis B vaccine shortly after birth. The CDC and some experts outside the government credit the vaccine with being behind a sharp decline in acute cases of hepatitis B.
“This disease has gone down in the United States thanks to the effectiveness of our current immunization program,” Dr. Cody Meissner, one of the ACIP members who voted not to change the current schedule, said on Thursday during the two-day meeting.
But the level of antibodies, one measure of effectiveness, in vaccinated people drops over time, and has been detected to be at low levels at older ages, particularly among children who received a shot early in life, Cynthia Nevison, a CDC contractor, told panel members. She cited several papers, including a 2016 study of adults and children in Alaska.
The CDC acknowledges on its website that antibodies in vaccinated persons wane over time but also says that immune memory holds up.
Nevison also noted that hepatitis B cases were already declining from a peak in 1985, when the universal birth dose was first introduced, contrary to a 1991 CDC publication that outlined why the hepatitis B campaign was being expanded to all newborns and stated that “selective vaccination of persons with identified risk factors ... has not lowered the incidence of hepatitis B.”

Retsef Levi, a member of the CDC's Advisory Committee on Immunization Practices, at the CDC headquarters in Atlanta, Ga., on Dec. 4, 2025. (Elijah Nouvelage/Getty Images)
Clinical Trials and Recommendations
Dr. Tracy Beth Hoeg, the new acting director of the Food and Drug Administration’s Center for Biologics Evaluation and Research, during the meeting took aim at the clinical trials that underpinned approval of the hepatitis B vaccines, noting they had no control groups at all and followed infants for only up to seven days.
“We would never approve a vaccine based on data like those today,” she said.
Post-licensure trials have also not used comparison groups that received a placebo, which means “we have a very low level of confidence in saying ... that the benefits outweigh the risks with the amount of data that we have,” she said.
Levi, a professor at the Massachusetts Institute of Technology, described the data as outrageous.
“As a father and as a scientist, I don’t know how we have the courage—based on such slim evidence—to come to parents and tell them that’s okay to give to your zero-day baby, especially when the risk is so low,” he said.
The CDC currently recommends that children receive an initial hepatitis B vaccine shortly after birth, another at 1 to 2 months of age, and a third between 6 months and 18 months of age. The CDC says that more than 90 percent of recipients younger than 40 develop antibodies after three doses, and estimates the regimen is 80 percent to 100 percent effective.
The CDC’s immunization schedule serves as guidance for states and organizations across the country. Many states mandate vaccinations based completely or largely on the schedule.
The current recommendation for infants to receive a dose of a hepatitis B vaccine within 24 hours of birth should remain in place for infants born to women who test positive for hepatitis B or whose hepatitis B status is unknown, ACIP members said in one of the votes.
For infants born to women who test negative, ACIP recommends individual-based decision-making, or not proceeding with vaccination unless parents consult with health care providers and consider the risks and benefits of the vaccine, and the risks of hepatitis B infection, the panel said.
Eight members voted in favor, and three voted against.
If parents proceed, the panel suggests an initial dose no earlier than 2 months of age.
For children who have received at least one dose, parents should talk with doctors about potentially testing their children for antibodies against hepatitis B before having them receive additional doses, ACIP said. It supports insurers covering the cost of the testing.

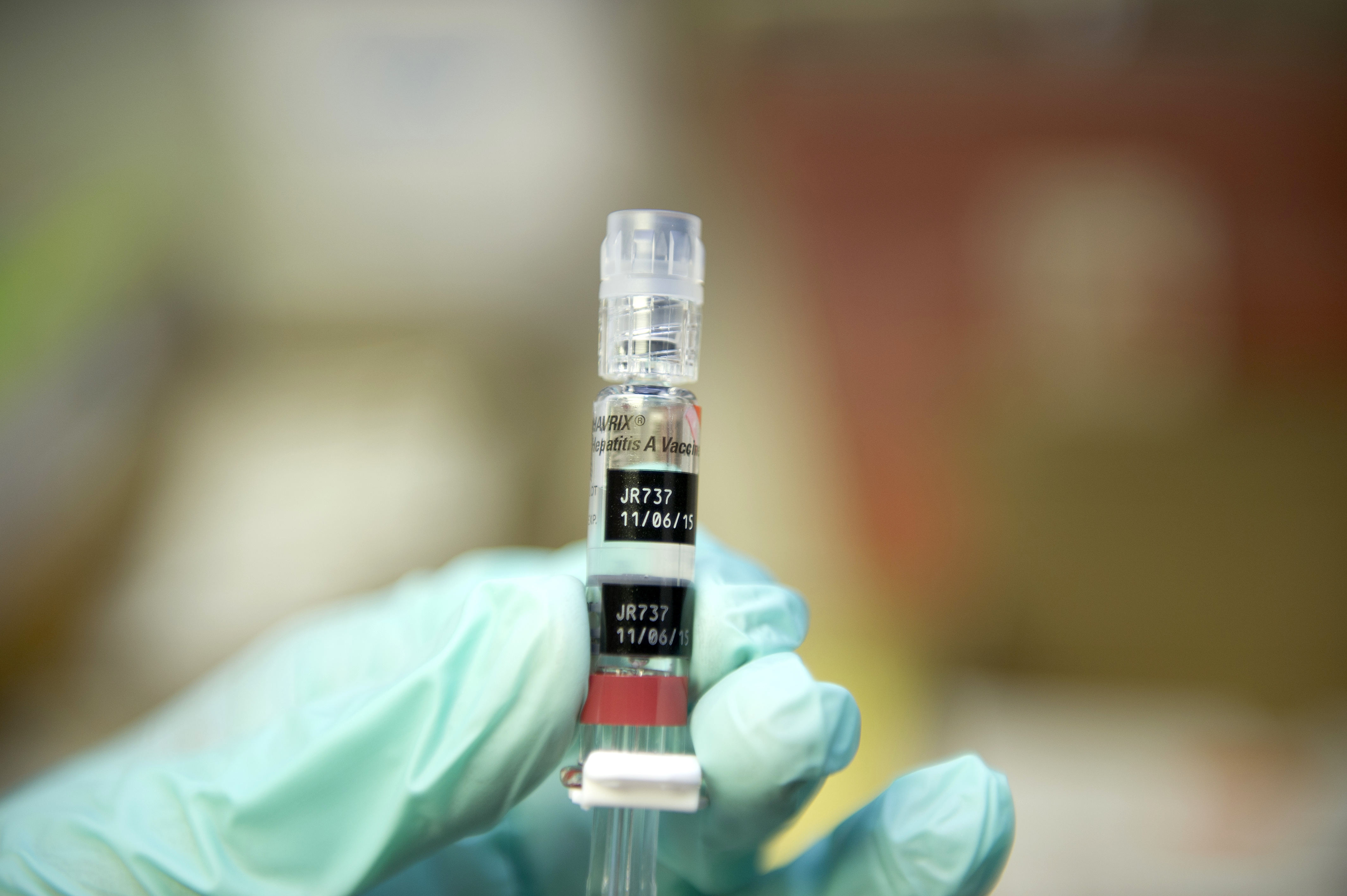
A baby after receiving a vaccine for hepatitis B and other diseases, in a file illustration photograph. (Riccardo Milani/Hans Lucas/AFP via Getty Images)
Opposition and Support
Outside groups such as the American Academy of Family Physicians and some former CDC officials were among those opposing a change in policy. Former CDC Director Dr. Rochelle Walensky and two other doctors estimated that there would be a higher number of hepatitis B infections among children from their mothers if the first dose was pushed back.
“Delaying the first hepatitis B vaccine dose beyond the newborn period introduces risks that have lifelong detrimental consequences and no measurable health benefit,” they said in an opinion article published by the Journal of the American Medical Association.
The CDC has not modeled the impact of delaying the first dose of hepatitis B vaccination, an HHS spokesperson told The Epoch Times in a recent email.
Children’s Health Defense, which was formerly chaired by Kennedy, and a number of other organizations supported updating the recommendations.
Brian Hooker, chief scientific officer of Children’s Health Defense, told The Epoch Times this week that babies should avoid the aluminum salts utilized as an adjuvant in the vaccine and that alternatives such as immunoglobulin are sufficient.
Vicky Pebsworth, an ACIP member who chairs the panel’s hepatitis B workgroup, said its review of the hepatitis B vaccine, which partially drove the discussion and votes, stemmed from the fact that the vaccine had not been reviewed for a long time, while ACIP’s charter says it will periodically review pediatric vaccines. She also cited parental surveys that found some parents avoided or delayed hepatitis B vaccination for their children due to concerns over safety and whether the vaccine was necessary. Adverse events following vaccination include fever and Guillain-Barré syndrome.
In many other high-income countries, officials only recommend hepatitis B vaccination early or at all to infants whose mothers tested positive for the virus.
Representatives of GlaxoSmithKline, Merck, and Sanofi, which manufacture hepatitis B vaccines, spoke in opposition to altering the schedule.
“Data consistently show that hepatitis B birth dose vaccination is critical in preventing chronic hepatitis B virus infections,” Dr. Candice Robinson, medical director of scientific affairs and public health at GlaxoSmithKline, told the panel.
If the CDC adopts the changes, it would be the latest update to the vaccine schedule under Kennedy’s leadership. Previous changes included removing the universal recommendation for COVID-19 vaccines and endorsing standalone vaccination against varicella, commonly known as chickenpox.